Starting anticoagulation
Check with local guidelines before prescribing.
Example guidance:
Enoxaparin therapy is given until adequate anticoagulation with warfarin is achieved. In situations where therapeutic anticoagulation with heparin is required and enoxaparin therapy is unsuitable (e.g. in renal impairment where CrCl < 30ml/min) then a heparin infusion may be required
- if there is a need for a heparin infusion then give heparin (25,000u/24h with 0.9% saline in a syringe pump). Monitor effects with kaolin-cephalin clotting time (aim for 1.5-2.5 times the control)
- for most indications UFH has been superseded by low molecular weight heparins (LMWHs), although UFH may be preferred where a more rapid onset of action is desirable, for example in high risk pulmonary embolism (1)
- after clinical assessment has demonstrated an indication for heparin treatment, the patient's medical and drug history should be assessed and baseline blood tests including platelet count, coagulation screen (in order to check baseline APTT ratio is normal), urea, electrolytes and liver function tests should be obtained. These may reveal contraindications or risk factors for bleeding, such as anaemia, thrombocytopenia, renal failure, or coagulopathy (eg due to severe liver disease)
- a baseline platelet count should be carried out for the assessment of possible subsequent development of heparin induced thrombocytopenia, an important complication of heparin use
- low-dose UFH (5,000 international units (IU) 8-12 hourly by subcutaneous injection), given as prophylaxis for venous thromboembolism, does not require monitoring of the APTT ratio; nor does low-dose infusion for prevention of clotting in peripheral arterial catheters (1)
If rapid anticoagulation is required warfarin should be initiated at a dose of 5 mg or 10 mg once a day for 2 days and re-measure the person's international normalized ratio (INR) on day three (2)
- however for people with atrial fibrillation there is no need to achieve anticoagulation rapidly; a slow-loading regimen is safe and achieves therapeutic anticoagulation in the majority of people within 3-4 weeks
The initial dosing regimen should be lower (5 mg) when there is increased sensitivity to warfarin (for example low body weight, drug therapy which increases warfarin sensitivity; for example some antibiotics, heart failure, liver failure, prolonged baseline prothrombin time)
- more cautious dosing should also be considered when warfarin is introduced within 7-10 days of surgery. Heparin prolongs the prothrombin time but in patients taking both heparin and warfarin at the start of treatment, the INR can be used for dosing warfarin without stopping heparin, provided that the APTT ratio is within or below the therapeutic range for heparin (1)
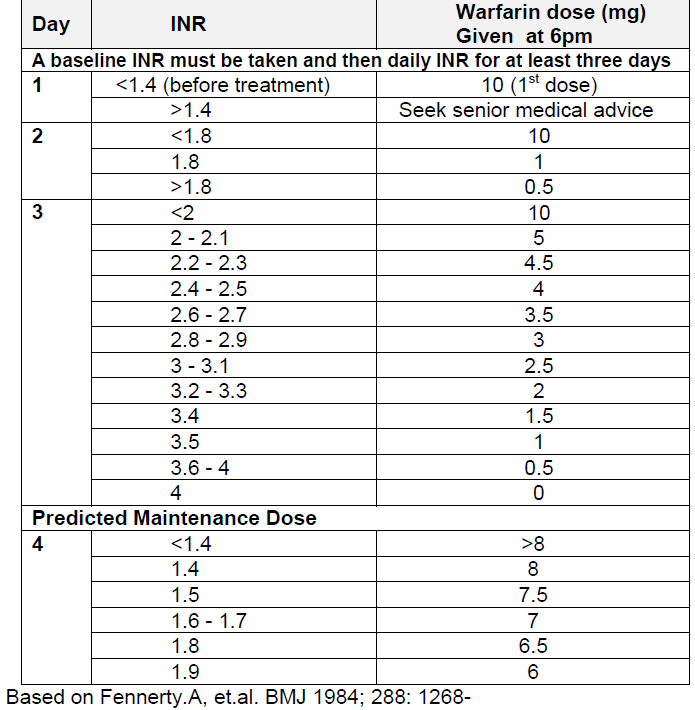
Warfarin takes about 3 days to work but can be started at the same time - this example table considers use of an initial 10mg dose (3,4)
Check for the following risk factors (3,4):
- Age>70 years
- Weight <60kg
- Liver impairment
- Increased bleeding risk (other causes)
- Low albumin <36g/L
- Parenteral feeding
- Interacting medications
- History of significant bleed
This regimen is recommended where rapid anticoagulation is desired AND the patient has no risk factors outlined above.
The heparin should be stopped when the INR is greater than 2.
INR monitoring (5):
- daily, or on alternate days, until it is within the therapeutic range (usually between 2.0 and 3.0, ideally 2.5) on two consecutive occasions
- note: although the INR may be measured each day after starting warfarin, a meaningful INR can only be obtained 3-4 days after starting treatment
- then, twice weekly for 1-2 weeks, followed by weekly measurements until at least two INR measurements are within the therapeutic range
- thereafter, depending on the stability of the INR, at longer intervals (for example, up to every 12 weeks, if agreed locally). Once a stable warfarin dose that controls the INR has been established, changes in dose are seldom required
The clotting laboratory should be informed that a patient is on both heparin and warfarin as the INR assay needs modification.
There are also regimens available for initiating anticoagulation in a community setting for patients with atrial fibrillation (4) - an example "slow start warfarin regime" is linked.
Notes (6):
- for outpatients who do not require rapid anticoagulation:
- a slow-loading regimen is safe and achieves therapeutic anticoagulation in the majority of patients within 3-4 weeks. This appears to avoid over-anticoagulation and bleeding associated with rapid loading
- for patients requiring rapid initiation of oral anticoagulation:
- regimens that start with 5 mg doses or a single 10 mg dose followed by 5 mg doses may be preferable to regimens that start with repeated 10 mg doses in certain patient groups, e.g. the elderly (>60 years of age), those with liver disease or cardiac failure and those at high risk of bleeding
NICE has updated its technological appraisal guidance for apixaban, dabigatran, edoxaban, and rivaroxaban for the prevention of stroke and systemic embolism in people with AF. Although the licensed indications have not changed, NICE now emphasise the importance of having an informed discussion on the relative risks and benefits of each DOAC before initiating treatment, and discussing the risks and benefits of switching from warfarin to a given DOAC, taking into account their level of INR control. before proceeding with a switch. (7,8,9,10)
Reference:
- SIGN Guideline 129.Antithrombotics: indications and management (last updated June 2013). Available: http://www.sign.ac.uk/assets/sign129.pdf
- Prescribers' Journal (1997), 37(3),173-9.
- Wirral University Teaching Hospital NHS Trust. Oral Anticoagulants (VKA and DOAC) Guidelines for prescribing, monitoring and management.
- Br J Clin Pharmacol 1998 Aug;46(2):157-61
- NHS Specialist Pharmacy Service (October 2017). Suggestions for Drug Monitoring in Adults in Primary Care
- Baglin TP et al. British Committee for Standards in Haematology - Guidelines on oral anticoagulation (warfarin): 4th edition - 2011 update (online).
- Apixaban for preventing stroke and systemic embolism in people with nonvalvular atrial fibrillation; NICE Technology Appraisal Guidance - last updated July 2021
- Dabigatran etexilate for the prevention of stroke and systemic embolism in atrial fibrillation; NICE Technology Appraisal Guidance - last updated July 2021
- Rivaroxaban for the prevention of stroke and systemic embolism in people with atrial fibrillation; NICE Technology Appraisal Guidance - last updated July 2021
- Edoxaban for preventing stroke and systemic embolism in people with non-valvular atrial fibrillation; NICE Technology Appraisal Guidance - last updated July 2021
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page