Warfarin slow start regime
Background
Patients not requiring rapid anticoagulation can be safely managed using a slow loading regimen which results in therapeutic anticoagulation within 3-4 weeks in the majority of patients. This appears to avoid over-anticoagulation and bleeding associated with rapid loading (1). This regimen is suitable for use in both the secondary and primary care setting and allows for induction of anticoagulation therapy requiring only weekly monitoring (1).
Indications:
For use in patients for whom immediate anticoagulation is not required. These include:
- chronic or paroxysmal atrial fibrillation;
- selected patients with left ventricular thrombus;
- selected patients with mitral stenosis;
- stroke outpatients in sustained AF who have waited 14 days following the acute event with a CT head scan that has excluded haemorrhage;
- selected patients with pulmonary hypertension.
Exclusion Criteria:
Patients requiring immediate anticoagulation. These include:
- deep vein thrombosis;
- pulmonary embolus;
- mechanical prosthetic cardiac valve insertion;
- arterial embolus;
- selected patients with atrial fibrillation, left ventricular thrombus, mitral stenosis;
- pulmonary hypertension associated with venous thromboembolic disease.
Aim: To initiate warfarin therapy with a target INR 2.5
Regimen:
- 1. Ensure the patient has no contraindications to warfarin and confirm with a senior member of the medical team that the slow start regimen is appropriate. Generally if a patient is taking aspirin, this should be continued until the INR is therapeutic then STOPPED.
- 2. Ensure baseline bloods (FBC, U&E, LFT, coagulation screen) are satisfactory. If in doubt, discuss with the patient's consultant. If baseline INR>1.2, seek haematology advice.
- 3. Explain to the patient the indication for warfarin treatment and the risks and benefits of it.
- 4. Prescribe 2mg of warfarin daily at 6pm for 1 week. For inpatients prescribe on the warfarin prescription and monitoring chart. Clearly mark the indication: Atrial Fibrillation Slow Start Regimen .
- 5. Repeat INR after 7 days of warfarin therapy.
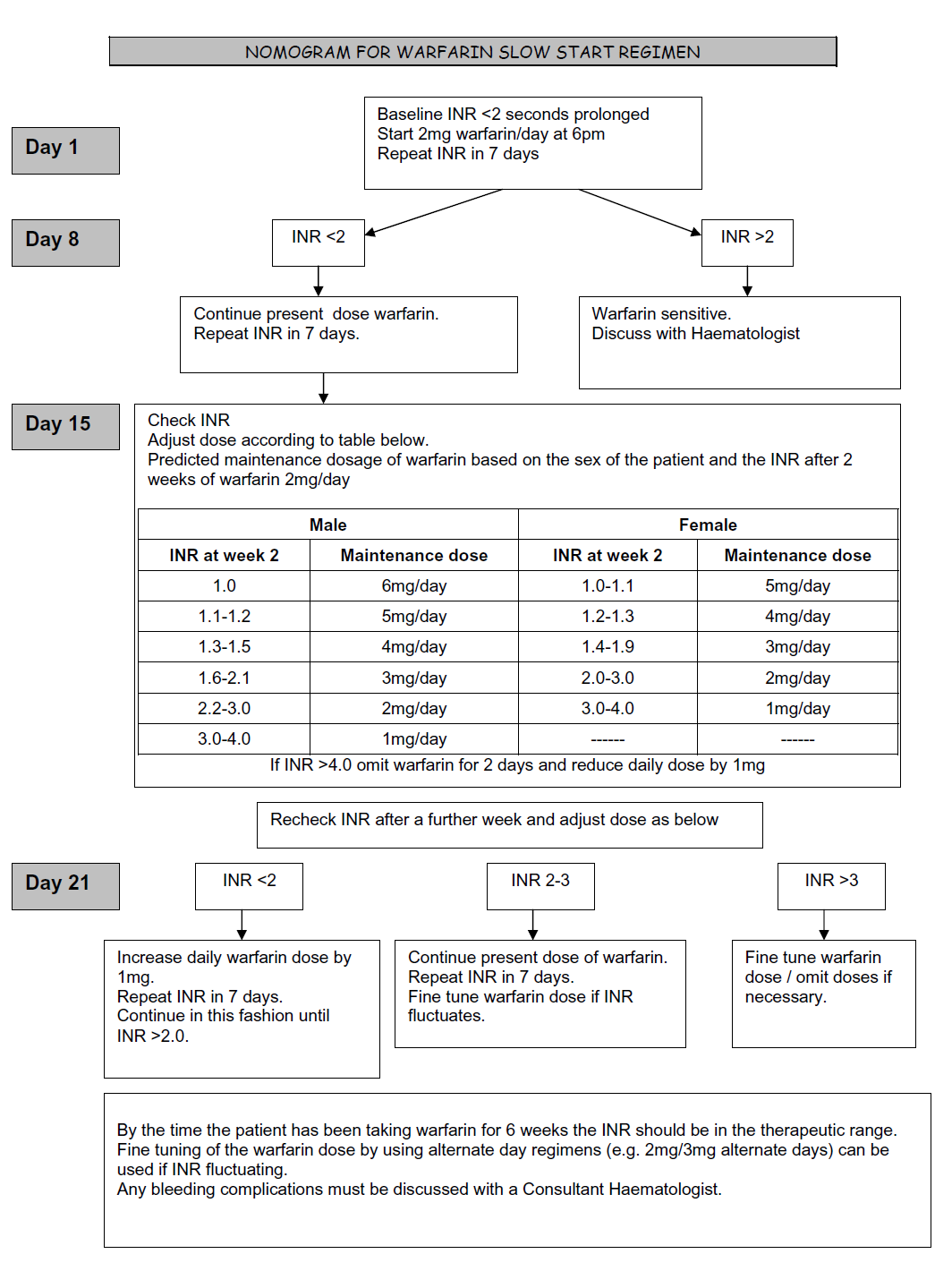
- 6. Adjust dose as per nomogram
- 7. In patients at discharge should be referred to the anticoagulant clinic using the Anticoagulation Referral Form, accompanied by a copy of the warfarin prescription chart(s)
Reference
- Guidelines on oral anticoagulation with warfarin, British Committee for Standards in Haematology (2011)
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page