Acute coronary syndrome (ACS)
Acute coronary syndromes due to ischaemic heart disease remain a significant cause of morbidity and mortality
- in England and Wales in July 2023, ischaemic heart disease was the leading cause of death in July 2023, with 77.0 deaths per 100,000 people in England and 85.8 deaths per 100,000 people in Wales (1) In Scotland, the leading cause of death in August 2023 was ischaemic heart disease, which accounted for 10% of all deaths (2).
- coronary heart disease is the single biggest cause of death in the UK as well as being a major cause of premature mortality (3)
- acute coronary syndrome (ACS) encompasses previous terms such as non-Q wave myocardial infarction and unstable angina (4)
- ACS is defined as:
- 1. unstable angina (symptoms at rest with ECG changes)
- 2. Non STEMI (non ST elevation myocardial infarction) with at least two of the following criteria
- symptoms at rest
- raised serum Troponin
- ECG changes
- 3. STEMI (ST elevation myocardial infarction) symptoms with ST elevation on ECG
- acute coronary syndromes encompass a spectrum of unstable coronary artery disease from unstable angina to transmural myocardial infarction
- all have a common aetiology in the formation of thrombus on an inflamed and complicated atheromatous plaque
- principles behind the presentation, investigation and management of these syndromes are similar with important distinctions depending on the category of acute coronary syndrome
Clinical presentation and immediate assessment
- patients with suspected acute coronary syndrome should be assessed immediately by an appropriate healthcare professional and a 12 lead electrocardiogram should be performed
- repeat 12 lead electrocardiograms should be performed if there is diagnostic uncertainty or a change in the clinical status of the patient, and at hospital discharge
- patients with persisting bundle branch block or ST segment change should be given a copy of their electrocardiogram to assist their future clinical management should they represent with a suspected acute coronary syndrome
Biochemical diagnosis
- in patients with suspected acute coronary syndrome, serum troponin concentration should be measured on arrival at hospital to guide appropriate management and treatment
- to establish a diagnosis in patients with an acute coronary syndrome, a serum troponin concentration should be measured 12 hours from the onset of symptoms
- to establish a diagnosis in patients with an acute coronary syndrome when symptom onset is uncertain, serum troponin concentration should be measured 12 hours from presentation
- when considering a diagnosis of ACS, serum troponin concentrations should not be interpreted in isolation but with regard to the clinical presentation of the patient
Management is guided based on whether STEMI or NSTEMI/unstable angina
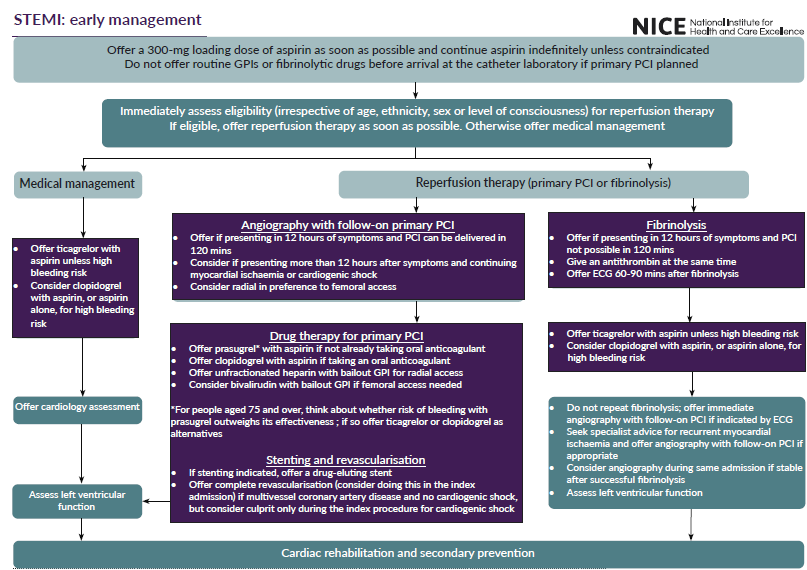
If STEMI:
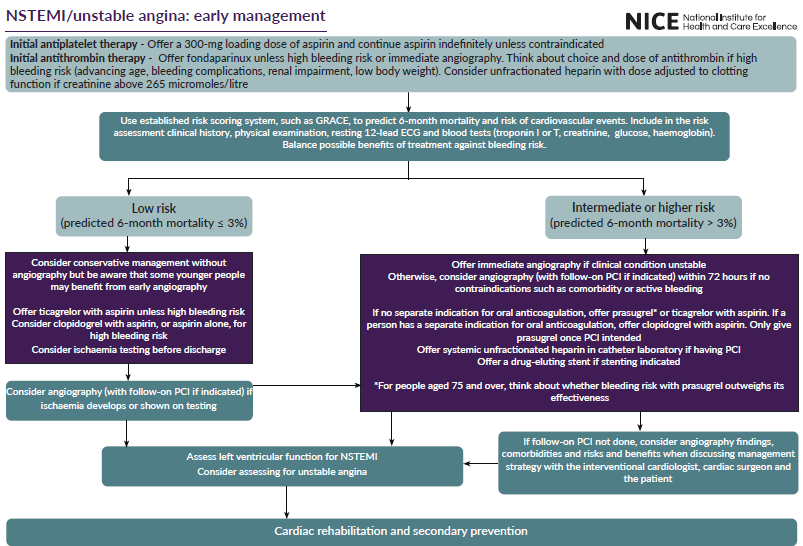
If NSTEMI/unstable angina:
A study investigating two-year mortality following diagnosis of acute coronary syndrome showed (4):
- mortality rate was 5.5% within two years of discharge
- independent mortality predictors identified were:
- age, low ejection fraction, no coronary revascularization/thrombolysis, elevated serum creatinine, poor EQ-5D score, low haemoglobin, previous cardiac or chronic obstructive pulmonary disease, elevated blood glucose, on diuretics or an aldosterone inhibitor at discharge, male sex, low educational level, in-hospital cardiac complications, low body mass index, ST-segment elevation myocardial infarction diagnosis, and Killip class
- independent mortality predictors identified were:
Data from a large Swedish registry including 108 315 post-MI patients with long-term follow-up revealed a cumulative rate of a cardiovascular composite endpoint (cardiovascular death, recurrent MI, and stroke) of 18.3% in the first year after MI, 9.0% in the subsequent year and 20.0% in the following 3 years (6)
ACS in premenopausal women (7)
- over the past 2 decades, rising hospitalization rates for acute myocardial infarction (MI) in younger women have been reported in the United States and other countries
- younger women less often receive guideline-directed medical therapies after presentation with an acute coronary syndrome (ACS), including lipid-lowering medications, nonaspirin antiplatelet agents, coronary angiography, and revascularization
- studies have shown worse outcomes for young women with ACS compared with young men, with some studies demonstrating that female sex is an independent predictor of mortality in younger patients with ACS
- compared with young men and postmenopausal women, including a relatively greater incidence of MI with no obstructive coronary arteries (MINOCA) and spontaneous coronary artery dissection (SCAD)
- whereas atherosclerotic disease (obstructive or nonobstructive) accounts for most presentations, a substantial number are attributable to nonatherosclerotic causes, including spontaneous coronary artery dissection, epicardial coronary artery spasm, and coronary embolism
References:
1. Office for National Statistics. Monthly mortality analysis, England and Wales: July 2023.
2. National Records of Scotland. Monthly Mortality Analysis. August 2023
3. Acute coronary syndrome. Scottish Intercollegiate Guidelines Network - SIGN (2016)
4. National Institute for Health and Care Excellence. Acute coronary syndromes. Nov 2020 [internet publication].
5. Pocock SJ et al. Predicting two-year mortality from discharge after acute coronary syndrome: An internationally-based risk score. Eur Heart J Acute Cardiovasc Care. 2019 Dec; 8(8):727-737.
6. Jernberg T, Hasvold P, Henriksson M, Hjelm H, Thuresson M, Janzon M. Cardiovascular risk in post-myocardial infarction patients: nationwide real world data demonstrate the importance of a long-term perspective. Eur Heart J. 2015;36:1163-1170.
7. Kovacic JC et al; American Heart Association Cardiovascular Interventions Committee of the Council on Clinical Cardiology and the Women’s Health Science Committee of the Council on Clinical Cardiology and Stroke Council; Council on Cardiovascular and Stroke Nursing; Council on Cardiovascular Surgery and Anesthesia; Council on Lifelong Congenital Heart Disease and Heart Health in the Young; and Council on Quality of Care and Outcomes Research. Acute Coronary Syndromes in Premenopausal Women: A Scientific Statement From the American Heart Association. Circulation. 2026 Feb 3.
Related pages
- Unstable angina
- Non-Q wave myocardial infarction (MI)
- Myocardial infarction
- Driving and cardiovascular disease (CVD)
- Immediate management of suspected acute coronary syndrome
- Assessment and diagnosis of recent onset chest pain or discomfort of suspected cardiac origin
- Assessment in hospital in patients with acute coronary syndrome
- Prognosis
- Killip classification of heart failure
- Working (returning to work and heart disease)
- Management post ACS in primary care
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.