Management post ACS in primary care
Assessment and Investigations:
- attitude and psychological state. Exercise and abilities and propensities. Dietary habits and knowledge
- smoking habits
- blood pressure
- full lipid profile (cholesterol will be lower than usual for 6 weeks post MI)
Management:
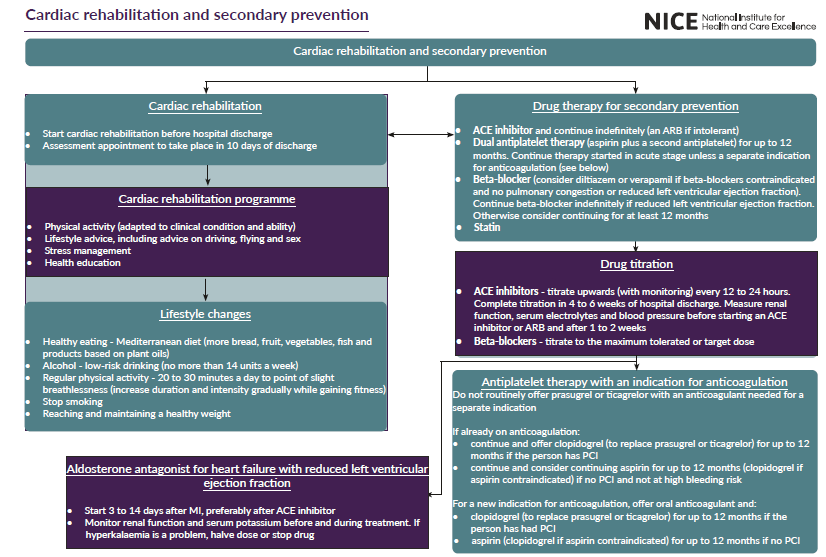
- cardiac rehabilitation
- stop smoking (record smoking status and advice)
- dietary advice with weight control if indicated
- control BP - treatment threshold is 140/90
A schemata has been suggested (1):
Medication Regimes: The following drug interventions work by independent mechanisms and their effects seem to be additive. All patients who have had an acute MI should be offered treatment with a combination of the following drugs (1):
- drug therapy
- offer all people who have had an acute MI treatment with the following drugs:
- ACE (angiotensin-converting enzyme) inhibitor
- dual antiplatelet therapy (aspirin plus a second antiplatelet agent)
- beta-blocker
- statin
- ensure that a clear management plan is available to the person who has had an MI and is also sent to the GP, including:
- details and timing of any further drug titration
- monitoring of blood pressure
- monitoring of renal function
- offer all people who have had an acute MI treatment with the following drugs:
- all people who have had an MI should be offered an assessment of bleeding risk at their follow-up appointment
- all people who have had an MI should be offered an assessment of left ventricular function
Notes:
- consider continuing a beta-blocker for 12 months after an MI for people without reduced left ventricular ejection fraction (1)
- do not offer people without left ventricular systolic dysfunction or heart failure, who have had an MI more than 12 months ago, treatment with a beta-blocker unless there is an additional clinical indication for a beta-blocker (1)
Reference:
- NICE (2020). Acute coronary syndromes. [NG185]
Related pages
- Trials of therapeutic intervention in MI
- Cholesterol measurement following myocardial infarction
- Secondary prevention of ischaemic heart disease
- Insulin therapy in type 2 diabetes post MI
- Lifestyle targets in prevention of coronary heart disease
- ACE inhibitors in myocardial infarction
- NICE guidance - antiplatelet therapy following myocardial infarction (MI)
- Beta-blockers in myocardial infarction
- Statins
- Calcium channel blockers in myocardial infarction
- Aldosterone antagonists in the management of heart failure
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.