The diagnosis of hypertension should not be made on the basis of a single elevated reading. In many cases, a second blood pressure reading is lower, and often, a third lower still.
Patients found to have malignant or accelerated phase hypertension should be managed as suggested below.
The majority of patients will have essential hypertension but it is nevertheless imperative to fully investigate for secondary causes.
Assessment should also consider other risk factors for cardiovascular disease and stroke.
Measuring blood pressure:
- because automated devices may not measure blood pressure accurately if there is pulse irregularity (for example, due to atrial fibrillation), palpate the radial or brachial pulse before measuring blood pressure. If pulse irregularity is present, measure blood pressure manually using direct auscultation over the brachial artery
- if using an automated blood pressure monitoring device, ensure that the device is validated and an appropriate cuff size for the person's arm is used
- in people with symptoms of postural hypotension (falls or postural dizziness):
- measure blood pressure with the person either supine or seated
- measure blood pressure again with the person standing for at least 1 minute prior to measurement
- if the systolic blood pressure falls by 20 mmHg or more when the person is standing:
- review medication
- measure subsequent blood pressures with the person standing
- consider referral to specialist care if symptoms of postural hypotension persist
Diagnosing hypertension
When considering a diagnosis of hypertension, measure blood pressure in both arms
- If the difference in readings between arms is more than 15 mmHg, repeat the measurements
- If the difference in readings between arms remains more than 15 mmHg on the second measurement, measure subsequent blood pressures in the arm with the higher reading
If blood pressure measured in the clinic is 140/90 mmHg or higher:
- take a second measurement during the consultation
- if the second measurement is substantially different from the first, take a third measurement. Record the lower of the last two measurements as the clinic blood pressure
If clinic blood pressure is between 140/90 mmHg and 180/120 mmHg, offer ambulatory blood pressure monitoring (ABPM) to confirm the diagnosis of hypertension. If a person is unable to tolerate ABPM, home blood pressure monitoring (HBPM) is a suitable alternative to confirm the diagnosis of hypertension
- see below for people with a clinic blood pressure 180/ 120mmHg or higher
Confirming the Diagnosis
- if the clinical BP is 140/90 mmHg or Higher, Offer ABPM to confirm the diagnosis
- if the patient is unable to tolerate ABPM, HBPM to confirm the diagnosis of HTN
- while waiting to confirm the diagnosis, carry out investigations for target organ damage and formal CVD assessment.
- CVD Assessment using a CVD assessment tool
- test for the presence of protein in the urine by sending a urine sample for estimation of the albumin: creatinine ratio and test for haematuria using a reagent strip
- take a blood sample to measure glycated haemoglobin (HbA1C), electrolytes, creatinine, estimated glomerular filtration rate, total cholesterol and HDL cholesterol
- examine the fundi for the presence of hypertensive retinopathy
- arrange for a 12-lead electrocardiograph to be performed
Ambulatory blood pressure monitoring
- when using ABPM to confirm a diagnosis of hypertension, ensure that at least two measurements per hour are taken during the person's usual waking hours (for example, between 08:00 and 22:00).
- use the average value of at least 14 measurements taken during the person's usual waking hours to confirm a diagnosis of hypertension
Home blood pressure monitoring
- When using home blood pressure monitoring (HBPM) to confirm a diagnosis of hypertension, ensure that:
- for each blood pressure recording, two consecutive measurements are taken, at least 1 minute apart and with the person seated and
- blood pressure is recorded twice daily, ideally in the morning and evening
- blood pressure recording continues for at least 4 days, ideally for 7 days
- discard the measurements taken on the first day and use the average value of all the remaining measurements to confirm a diagnosis of hypertension
Identifying who to refer for same-day specialist review
- if a person has severe hypertension (clinic blood pressure of 180/120 mmHg or higher), but no symptoms or signs indicating same-day referral
- carry out investigations for target organ damage as soon as possible:
- if target organ damage is identified, consider starting antihypertensive drug treatment immediately, without waiting for the results of ABPM or HBPM
- if no target organ damage is identified, repeat clinic blood pressure measurement within 7 days
- refer people for specialist assessment, carried out on the same day, if they have a clinic blood pressure of 180/120 mmHg and higher with:
- signs of retinal haemorrhage or papilloedema (accelerated hypertension) or
- life-threatening symptoms such as new onset confusion, chest pain, signs of heart failure, or acute kidney injury
- carry out investigations for target organ damage as soon as possible:
- refer people for specialist assessment, carried out on the same day, if they have suspected phaeochromocytoma (for example, labile or postural hypotension, headache, palpitations, pallor, abdominal pain or diaphoresis)
Stage 1 hypertension
- Clinic blood pressure ranging from 140/90 mmHg to 159/99 mmHg and subsequent ABPM daytime average or HBPM average blood pressure ranging from 135/85 mmHg to 149/94 mmHg.
Stage 2 hypertension
- Clinic blood pressure of 160/100 mmHg or higher but less than 180/120 mmHg and subsequent ABPM daytime average or HBPM average blood pressure of 150/95 mmHg or higher.
Stage 3 or severe hypertension
- Clinic systolic blood pressure of 180 mmHg or higher or clinic diastolic blood pressure of 120 mmHg or higher.
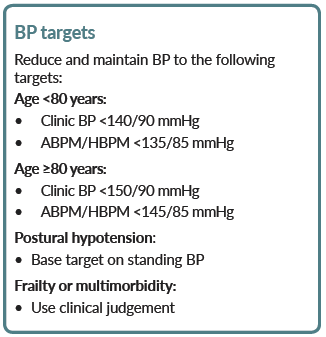
- in people with CKD and diabetes, and also in people with an ACR of 70 mg/mmol or more, aim to keep the systolic blood pressure below 130 mmHg (target range 120-129 mmHg) and the diastolic blood pressure below 80 mmHg.
Reference:
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.