Psoriasis is a common chronic skin disease characterised by cutaneous inflammation and epidermal hyperproliferation - lesions appear on any part of the skin, but particularly the scalp, sacral area, and over the extensor aspect of the knees and elbows
- the major manifestation of psoriasis is the chronic skin disease (although psoriatic joint disease is another major morbidity associated with psoriasis)
- psoriatic skin disease is characterised by cutaneous inflammation and epidermal hyperproliferation (normally cells of the epidermal layer renew every 28 days, but in psoriasis the regeneration occurs every 2 to 4 days) (1,2)
- lesions appear on any part of the skin, but particularly the scalp, lumbosacral area and over the extensor aspect of the knees and elbows (3).
- Characteristically, there are:
- well-defined, raised, erythematous and scaly lesions (3), which are "salmon pink" or "full rich red" in colour
- surface silvery scale which may be easily removed often leading to pin - point capillary bleeding (Auspitz sign) (4)
- they may or may not itch but this is not usually a prominent feature
- Characteristically, there are:
- lesions appear on any part of the skin, but particularly the scalp, lumbosacral area and over the extensor aspect of the knees and elbows (3).
- acute disease may manifest as inflammation and erythema while chronic lesions present as typical plaques (4). In most of the patients psoriasis presents in a chronic course with periods of remission (1).
- psoriasis is an emotionally and physically debilitating disease which is often underestimated by medical practioners (4)
A strong genetic predisposition can be seen in psoriasis. Around 8 genetic susceptibility loci (PSORS I-VIII) have been observed (1). Psoriasis susceptibility 1 (PSORS1) locus located on the 6th chromosome is considered to be the most important one and can be seen in up to 50% of psoriasis cases (3).
NICE suggest (4):
- psoriasis is an inflammatory skin disease that typically follows a relapsing and remitting course - prevalence of psoriasis is estimated to be around 1.3-2.2% in the UK.
- is uncommon in children (0.71%) and the majority of cases occur before 35 years
- is associated with joint disease in a significant proportion of patients (reported in one study at 13.8%)
- plaque psoriasis is characterised by well-delineated red, scaly plaques that vary in extent from a few patches to generalised involvement
- by far the most common form of the condition (about 90% of people with psoriasis)
- other types of psoriasis include guttate psoriasis and pustular (localised or generalised) forms
- distinctive nail changes occur in around 50% of all those affected and are more common in people with psoriatic arthritis
- several studies have also reported that people with psoriasis, particularly those with severe disease, may be at increased risk of cardiovascular disease, lymphoma and non-melanoma skin cancer
- therapeutics:
- first-line therapy describes traditional topical therapies (such as corticosteroids, vitamin D and vitamin D analogues, dithranol and tar preparations)
- second-line therapy includes the phototherapies (broad- or narrow-band ultraviolet B light and psoralen plus UVA light [PUVA]) and systemic non-biological agents such as ciclosporin, methotrexate and acitretin
- third-line therapy refers to systemic biological therapies such as the tumour necrosis factor antagonists adalimumab, etanercept and infliximab, and the monoclonal antibody ustekinumab that targets interleukin-12 (IL-12) and IL-23
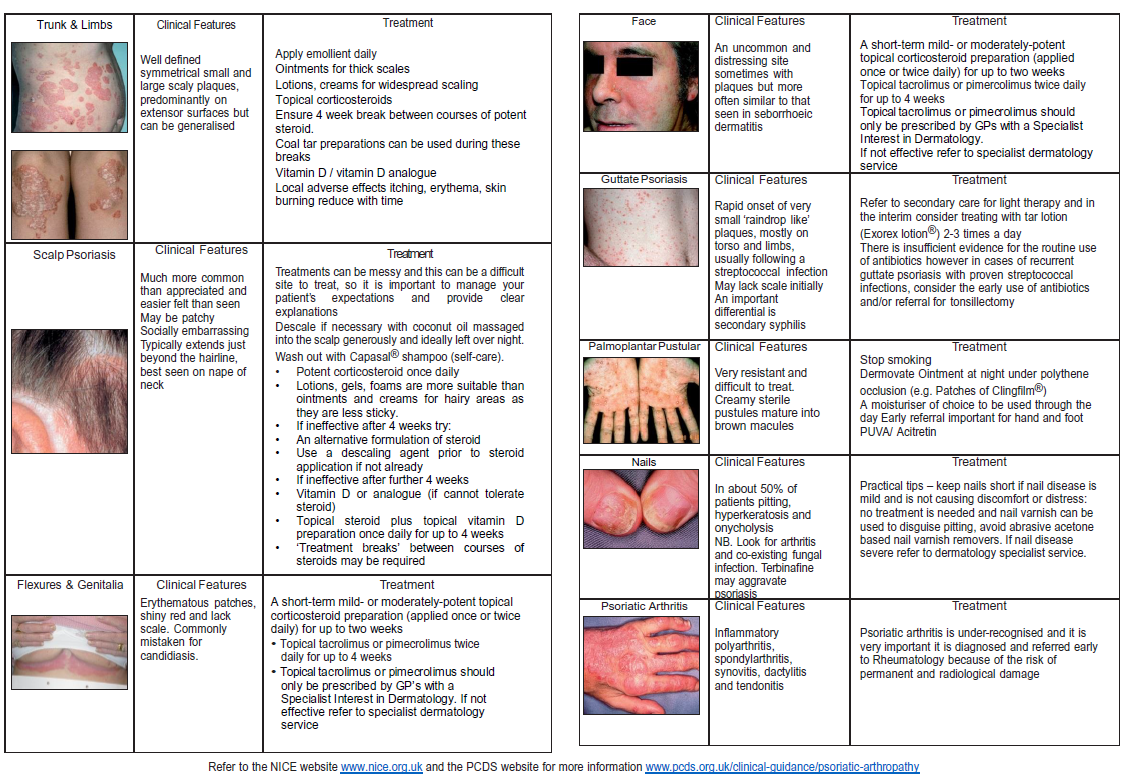
A useful summary algorithm based on NICE guidance for management of psoriasis in adults has been produced (5). This is an excellent summary for management in primary care:
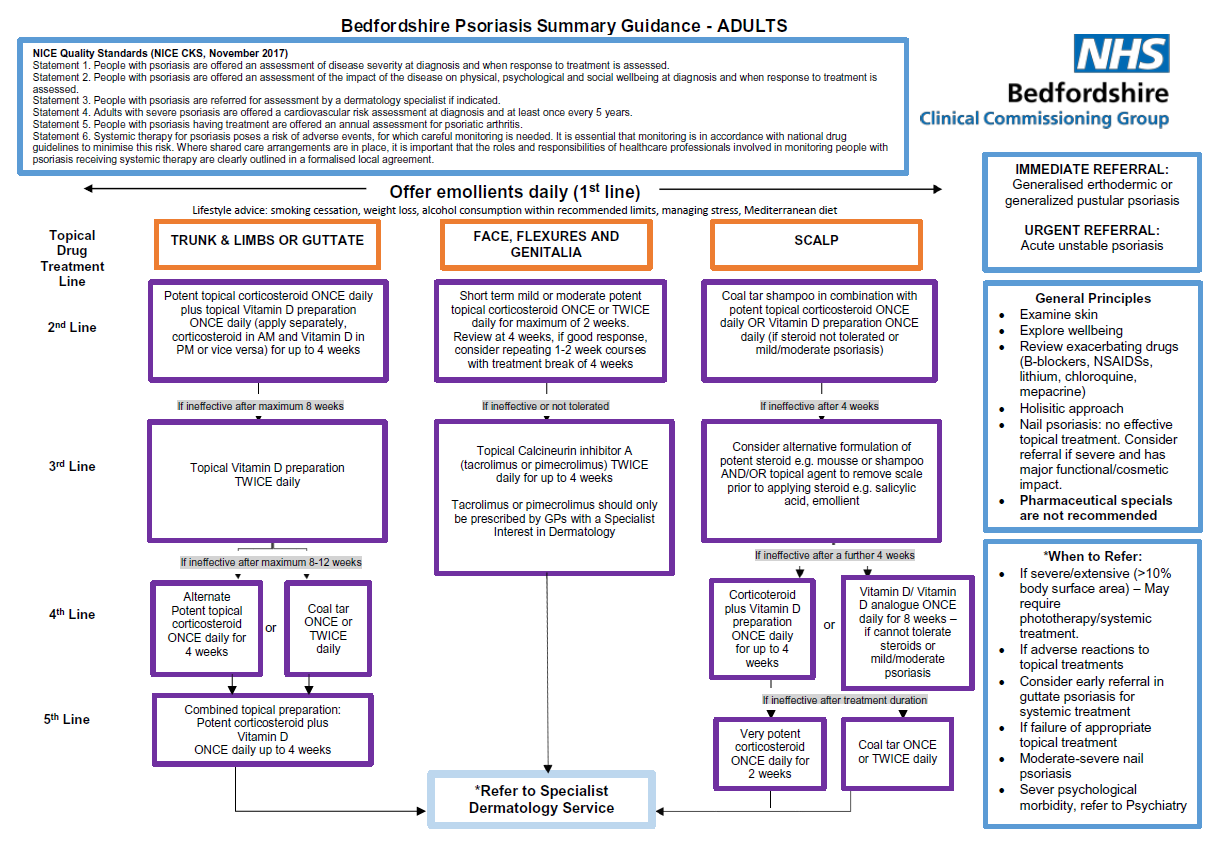
Notes (5):
Mild steroid cream/ointment | Hydrocortisone 1% (cream/ ointment) | Children: Any area up to twice a day Adults: Any area up to twice a day |
Moderate steroid cream/ointment | Clobetasone butyrate 0.05% (cream/ointment) (Eumovate (R) | Children: Up to twice a day. Face and flexures for severe flares max 3-5 days then reduce potency. Adults: all areas max twice a day |
Moderate steroid cream/ointment | Betamethasone valerate 0.025% (cream/ointment) | Children: Up to twice a day. Avoid face and flexures. Adults: all areas max twice a day |
Potent* steroid cream/ointment | Betamethasone valerate 0.1% (cream/ointment) | Children: Age <12 months: specialist initiation only Age>12 months: Short term use up to 14 days in areas like axilla and groin. Only if inadequate response to moderate steroid. Adults: body, limbs, feet and hands ONLY up to twice a day for max 7-14 days then reduce strength |
Potent* steroid cream/ointment | Mometasone furoate 0.1% (cream/ointment) [Elocon (R)] | Children: Only use if inadequate response to moderate steroid and when recommended by specialist in <12 months age. Use least amount possible once a day for no more than 5 days. Adults: Thin film of cream or ointment should be applied to affected areas once daily. If used on face, then max 5 days |
Very potent* steroid cream/ointment | Clobetasol proprionate 0.05% (cream/ointment) | Children: Never use without specialist advice. Adults: Never for face. Only for those unresponsive to potent steroids for a short course especially on hands or feet |
Key points when prescribing topical steroids:
- ointments should be used in the first instance if cosmetically acceptable. Creams contain more water and therefore may contain more preservatives - but they may be more cosmetically acceptable
- *there should be a four week gap between courses of potent/very potent steroid treatments
- refer to relevant product SPC (www.medicines.org.uk) for further information on side effects and excipients
Reference:
- 1. American Academy of Dermatology 2008. Guidelines of care for the management of psoriasis and psoriatic arthritis - Section 1. Overview of psoriasis and guidelines of care for the treatment of psoriasis with biologics
- 2. American Academy of Dermatology. Psoriasis
- 3. Schon M.P, Boehncke W.H. Psoriasis. NEJM 2005;352:1899-1912.
- 4. Guillen S, Khachemaoune A. Photo quiz - Large, Silvery Plaques. AFP 2007;75(8)
- 4. NICE (September 2017). Psoriasis - the assessment and management of psoriasis
- 5. NHS Bedfordshire Clinical Commissioning Group. Bedfordshire Psoriasis Summary Guidance - adults (Accessed 21/8/2019).
Related pages
- Epidemiology of psoriasis
- Pathogenesis of psoriasis
- Aetiology of psoriasis
- Clinical types of psoriasis
- Diagnosis of psoriasis - general principles
- General approaches to psoriasis treatment
- Prognosis
- Referral criteria from primary care - psoriasis
- Psoriasis and pregnancy
- PASI (psoriasis area and severity index)
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.