Vitamin D
Consult expert advice and local guidance.
Vitamin D consists of fat-soluble compounds with similar activity on calcium and phosphate physiology: enhancement of gastrointestinal absorption and an increase in bone deposition
- major biological functions of vitamin D are to regulate calcium and phosphate absorption and metabolism, and to maintain plasma calcium levels via bone resorption and formation
- these actions help to form and maintain healthy bones
- observational studies suggest that vitamin D also helps to maintain a healthy immune system and regulate cell growth and differentiation, to protect against certain cancers
Agents include:
- vitamin D2 - ergocalciferol
- pro-vitamin D3 - 7-dehydrocholesterol
- vitamin D3 - cholecalciferol
- 25-hydroxycholecalciferol - 25-HCC - calcidiol
- 1,25-dihydroxycholecalciferol - 1,25-DHCC - calcitriol
Key recommendations:
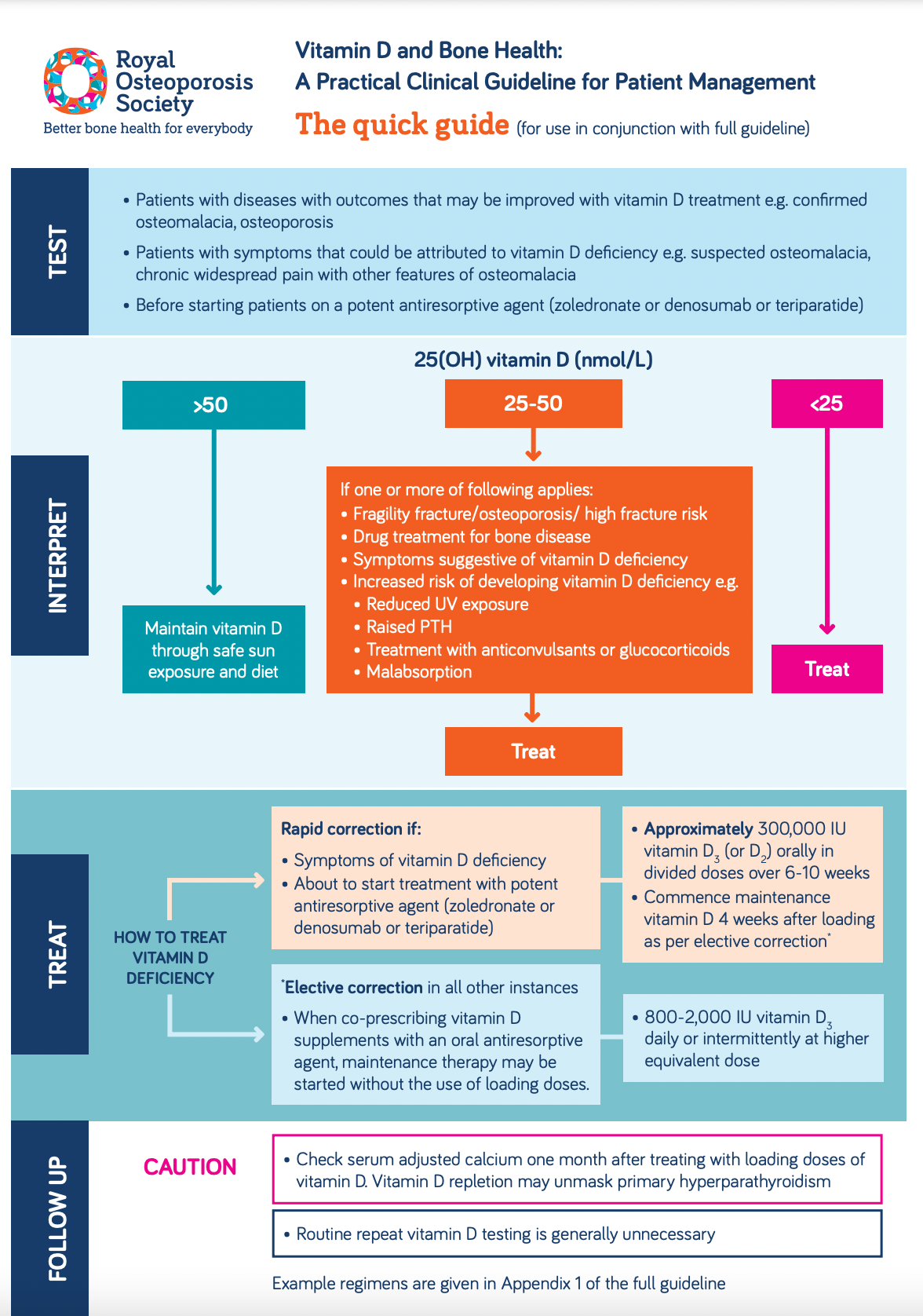
- measurement of plasma 25(OH)D is the best way of estimating vitamin D status (1):
- plasma 25(OH)D measurement is recommended for:
- patients with musculoskeletal symptoms that could be attributed to vitamin D deficiency
- patients suspected of having bone diseases that may be improved with vitamin D treatment
- patients with bone diseases, prior to specific treatment where correcting vitamin D deficiency may be necessary
- plasma 25(OH)D measurement is recommended for:
- routine monitoring of plasma 25(OH)D is generally unnecessary but may be appropriate in patients with symptomatic vitamin D deficiency or malabsorption and where poor compliance with medication is suspected (1)
- in most cases routine vitamin D testing is unnecessary in patients with osteoporosis or fragility fracture, who may be co-prescribed vitamin D supplementation with an oral antiresorptive treatment (1)
- where rapid correction of vitamin D deficiency is required, such as in patients with symptomatic disease or about to start treatment with a potent antiresorptive agent (zoledronate or denosumab or teriparatide), the recommended treatment regimen is based on fixed loading doses followed by regular maintenance therapy (1):
- a loading regimen to provide a total of approximately 300,000 IU vitamin D, given either as separate weekly or daily doses over six to ten weeks
- maintenance therapy comprising vitamin D in doses equivalent to 800-2,000 IU daily (occasionally up to a maximum of 4,000 IU daily), given either daily or intermittently at higher doses
- where correction of vitamin D deficiency is less urgent and when co-prescribing vitamin D supplements with an oral antiresorptive agent, maintenance therapy may be started without the use of loading dose (1)
Treatment of vitamin D deficiency in adults (1):
- the following adult vitamin D thresholds are adopted by UK practitioners in respect to bone health:
- plasma 25(OH)D <25 nmol/L is deficient
- plasma 25(OH)D of 25-50 nmol/L may be inadequate in some people
- plasma 25(OH)D > 50 nmol/L is sufficient for almost the whole population
- treatment thresholds (1):
- plasma 25OHD < 25 nmol/L: treatment recommended
- plasma 25OHD 25-50 nmol/L: treatment is advised in patients with the following:
- fragility fracture, documented osteoporosis or high fracture risk
- treatment with antiresorptive medication for bone disease
- symptoms suggestive of vitamin D deficiency
- increased risk of developing vitamin D deficiency in the future because of reduced exposure to sunlight, religious/cultural dress code, dark skin, etc.
- raised PTH
- medication with antiepileptic drugs or oral glucocorticoids
- plasma 25OHD > 50 nmol/L: provide reassurance and give advice on maintaining adequate vitamin D levels through safe sunlight exposure and diet
- plasma 25OHD < 25 nmol/L: treatment recommended
- oral vitamin D3 (cholecalciferol) is the treatment of choice in vitamin D deficiency (1)
- where rapid correction of vitamin D deficiency is required, such as in patients with symptomatic disease or about to start treatment with a potent antiresorptive agent (zoledronate or denosumab), the recommended treatment regimen is based on fixed loading doses followed by regular maintenance therapy:
- a loading regimen to provide a total of approximately 300,000 IU vitamin D, given either as separate weekly or daily doses over 6 to 10 weeks
- maintenance therapy comprising vitamin D in doses equivalent to 800-2000 IU daily (occasionally up to 4,000 IU daily), given either daily or intermittently at higher doses
- 1) Loading regimens for treatment of deficiency up to a total of approximately 300,000 IU given either as weekly or daily split doses. The exact regimen will depend on the local availability of vitamin D preparations but will include:
- 50,000 IU (tablets, capsules, or liquid), one given weekly for six weeks (300,000 IU)
- 40,000 IU capsules, given weekly for seven weeks (280,000 IU)
- 1,000 IU tablets, four a day given for 10 weeks (280,000 IU)
- 800 IU capsules, five a day for 10 weeks (280,000 IU)
- the following should be borne in mind:
- supplements should be taken with food to aid absorption
- calcium/vitamin D combinations should not be used as sources of vitamin D for the above regimens, given the resulting high dosing of calcium
- 2) Maintenance regimens may be considered 1 month after loading with doses equivalent to 800 to 2000 IU daily (occasionally up to 4,000 IU daily), given either daily or intermittently at a higher equivalent dose.
Monitoring:
All patients receiving pharmacological doses of vitamin D should have their plasma-calcium concentration checked at appropriate intervals relative to the indication and dosage, or where clinical symptoms indicate (3).
- Adjusted plasma calcium is recommended to be checked 1 month after completing the loading regimen or after starting vitamin D supplementation in case primary hyperparathyroidism has been unmasked (1)
- the presence of hypercalcemia ought to lead to cessation of further vitamin D supplementation prior to investigation of the hypercalcemia
- the presence of hypercalcemia ought to lead to cessation of further vitamin D supplementation prior to investigation of the hypercalcemia
- Vitamin D levels do not need to be checked routinely, and can take 3-6 months to reach a steady state after treatment has started (2)
- recheck vitamin D levels 6 months after a loading regimen of vitamin D has been given. If levels are still sub-optimal, compliance with medication should be discussed. Alternatively, consider referral to an appropriate specialist
Notes:
- dose conversion (2):
- the dose of vitamin D in micrograms can be calculated by dividing the number of international units by 40. Vitamin D2 (ergocalciferol) and vitamin D3 (colecalciferol) are considered equal in potency
- although there are suggestions that the onset of action of vitamin D3 is quicker
- for vegans, vitamin D2 (ergocalciferol) products which are derived from plants will be most suitable (2)
- however, prescribers will also need to check the formulation of the product (e.g. some ergocalciferol products will be formulated in a gelatine capsule, which will be unacceptable to vegans).
- however, prescribers will also need to check the formulation of the product (e.g. some ergocalciferol products will be formulated in a gelatine capsule, which will be unacceptable to vegans).
- calcium and vitamin D combined supplements are not routinely indicated in patients with low vitamin D3 levels unless the patient also has hypocalcaemia. The calcium component may be unnecessary and can reduce compliance due to unpalatability. Serum calcium levels should, however, be monitored (2)
- short acting potent analogues of vitamin D such as alfacalcidol or calcitriol should NOT be used in this situation because there is no evidence to support efficacy and it can lead to hypercalcaemia
- WARNING: NUT/SOYA ALLERGIES
- vitamin D preparations such dekristol and Fultium D3 contain peanut oil; Drisdol, Calceos and Adcal D3 contain soybean oil. For full details of excipients, refer to individual SPCs
- breast milk from women taking pharmacological doses of vitamin D may cause hypercalcemia if given to an infant (4)
- over-the-counter preparations (e.g. capsules, liquids) of cod or halibut liver oils are available and contain 2.5-20µg (100-800 IU) doses of vitamin D
- vitamin D supplementation is contraindicated in patients with hypercalcaemia or metastatic calcification
- relative contraindications include primary hyperparathyroidism, renal stones and severe hypercalciuria
- patients with mild to moderate renal failure or known to have mild hypercalciuria should be supervised carefully when taking vitamin D In patients with a history of renal stones, urinary calcium excretion should be measured to exclude hypercalciuria, a problem which requires specialist referral
- assessment of improvement in vitamin D (25OHD) status on replacement therapy (1)
- routine monitoring of serum 25OHD is generally unnecessary but may be appropriate in patients with symptomatic vitamin D deficiency or malabsorption and where poor compliance with medication is suspected.
- there is considerable variability between the results of studies examining the dose response to vitamin D supplementation, but it appears that much of this inconsistency results from the confounding effects of UV exposure in the summer months. When consideration is confined to the results of studies that examined the effect of supplementation on winter 25OHD levels, the results are more consistent:
- a daily supplement of 20 to 25 µg (800 to 1000 IU) calciferol will cause an increase in 25OHD of 24 to 29 nmol/L. Most of these studies have suggested that a new steady-state 25OHD level is reached by about 3 months and possibly not until 6 months.
- "..accordingly, it is a waste of resources to measure vitamin D levels too soon after the therapy has started. A minimum of 3 months treatment must be given and it may be more prudent to wait until 6 months have passed..."(1)
- specialist supervision in vitamin D supplementation (1)
- if a patient has tuberculosis or sarcoidosis
- patients with granulomatous disease are at risk of hypercalcaemia because of increased 1alpha-hydroxylase activity (which converts 25OHD to active 1,25(OH)2D). Toxicity has been reported during vitamin D treatment of tuberculosis and in patients with active sarcoidosis. specialist advice should be sought before starting these patients on vitamin D therapy
- there may be sub-groups of patients identified who are unable to maintain adequate vitamin D status. These may require a more aggressive replacement or maintenance schedule provided under specialist supervision in a secondary-care setting
- local guidance suggests seeking specialist advice for severe renal impairment (eGFR<30ml/min), pregnancy, hyperparathyroidism, or Paget’s disease (2)
- if a patient has tuberculosis or sarcoidosis
- children from age 1 year and adults need 10 µg (400IU) of vitamin D a day; this includes pregnant and breastfeeding women, and people at risk of vitamin D deficiency
- babies up to age of 1 year need 8.5 to 10 µg of vitamin D a day (5)
Reference:
- Royal Osteoporosis Society (2020). Vitamin D and Bone Health: A Practical Clinical Guideline for Patient Management.
- NHS Coventry and Warwickshire (2020). Vitamin D Prescribing Guidelines – Adults. Accessible at https://www.covwarkformulary.nhs.uk/docs/chapter09/CG019-Vitamin%20D%20Guidelines.pdf (accessed 16 May 2022)
- Specialist Pharmacy Service. Safety considerations when using Vitamin D. Available at: https://www.sps.nhs.uk/articles/safety-considerations-when-using-vitamin-d/#id-monitoring (accessed 24 June 2024)
- Primary vitamin D deficiency in adults Drug and Therapeutics Bulletin 2006;44:25-29
- NHS (2020). Vitamin D. Available at https://www.nhs.uk/conditions/vitamins-and-minerals/vitamin-d/ (accessed 16 May 2022)
Related pages
- Sources of vitamin D
- Interaction of some drugs and vitamin D supplementation
- Maintenance therapy following vitamin D supplementation
- Vitamin D metabolism
- Vitamin D physiology
- Vitamin D deficiency
- Vitamin D excess
- Role in other disease processes
- Possible non-adherance to vitamin D supplementation
- Recommended daily intake of vitamin D
- Vitamin D supplementation and risk of vitamin D excess (toxicity)
- Vitamin D and marine omega 3 fatty acid supplementation and incident autoimmune disease
- Vitamin D and development of diabetes mellitus
- Vitamin D supplementation and fracture risk in healthy adults
- Vitamin D and cancer
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.