Tetanus - prone injuries
Tetanus-prone wounds include:
- puncture-type injuries acquired in a contaminated environment and likely therefore to contain tetanus spores e.g. gardening injuries
- wounds containing foreign bodies
- compound fractures
- wounds or burns with systemic sepsis
- certain animal bites and scratches - although smaller bites from domestic pets are generally puncture injuries animal saliva should not contain tetanus spores unless the animal has been routing in soil or lives in an agricultural setting
Note: individual risk assessment is required and this list is not exhaustive e.g. a wound from discarded needle found in a park may a tetanus-prone injury but a needle stick injury in a medical environment is not
High-risk tetanus-prone wounds include: Any of the above with either:
- heavy contamination with material likely to contain tetanus spores e.g. soil, manure
- wounds or burns that show extensive devitalised tissue
- wounds or burns that require surgical intervention that is delayed for more than six hours are high risk even if the contamination was not initially heavy
Thorough cleaning of wounds is essential.
The rationale for using intramuscular tetanus immunoglobulin (IM-TIG) is to sufficiently and rapidly raise antibody levels in exposed individuals with antibody levels below the protective threshold, and who are not expected to make a sufficiently rapid memory response to vaccination
- median incubation period for tetanus is reported as 7 days but can range from 4-21 days and therefore it is important that either IM-TIG administration or active boosting occurs promptly following an exposure
- peak levels are achieved 4 days after an IM-TIG dose
- in individuals who receive a vaccine booster after having completed a full primary course, a measurable increase in antibody titres has been observed as early as 4 days, and levels increase substantially from day 7
- antibody levels achieved 5-7 days after a reinforcing dose of vaccine likely exceeds the estimated antibody boost from a prophylactic dose of IM-TIG in an adult
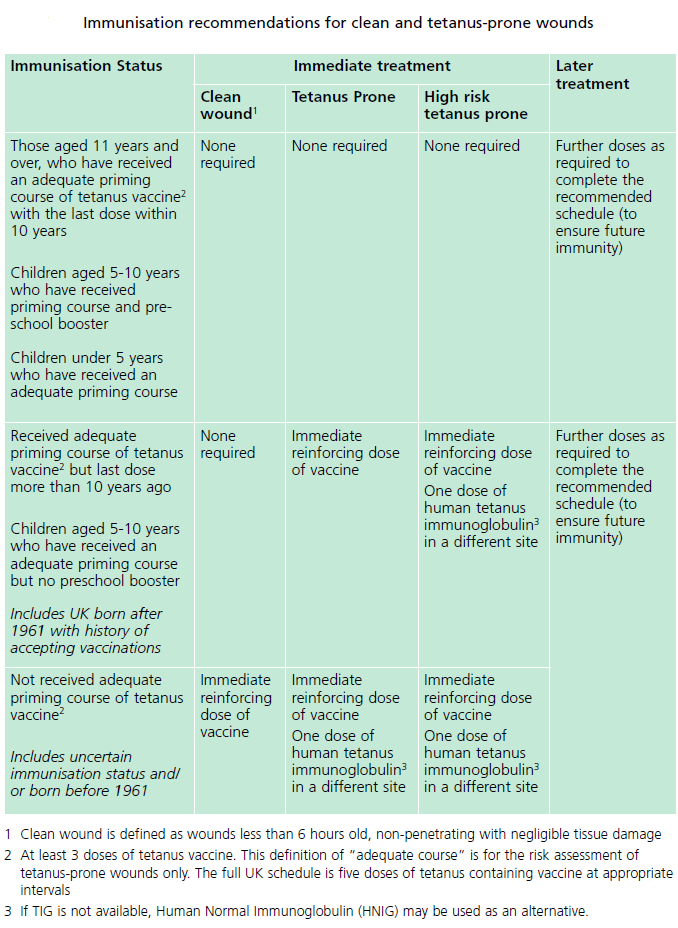
When a vaccine booster and/or IM-TIG is required
- recommendations are based on what would be considered an adequate priming course (defined as receiving at least 3 doses of tetanus vaccine at appropriate intervals)
- if adequate priming course then these individuals would be expected to retain antibody levels above the protective threshold for between 5 to 10 years (depending on the age at which they received their last dose)
- such individuals would be expected to have adequate protection following a tetanus prone injury and therefore not require any immediate treatment, but may need further doses of vaccine as required to complete the recommended schedule
- such individuals would be expected to have adequate protection following a tetanus prone injury and therefore not require any immediate treatment, but may need further doses of vaccine as required to complete the recommended schedule
- Individuals who have received an adequate priming course but are more than 5-10 years since the last dose (depending on the age of the final dose)
- would be expected to make a rapid response to a booster dose of vaccine and so all individuals in this group are recommended a booster dose of vaccine for immediate protection
- likely to be sufficient except in situations of heavy contamination and therefore, only individuals who have sustained a high risk injury require IM-TIG
- further doses of vaccine may be required to complete the recommended schedule for future immunity
- would be expected to make a rapid response to a booster dose of vaccine and so all individuals in this group are recommended a booster dose of vaccine for immediate protection
- for individuals who have not received an adequate priming course, any tetanus prone injury
- should receive both IM-TIG and a reinforcing dose of vaccine
- should include individuals with an uncertain immunisation status and /or those born before routine immunisation in 1961
- further doses of vaccine will be required to complete the recommended schedule
- if adequate priming course then these individuals would be expected to retain antibody levels above the protective threshold for between 5 to 10 years (depending on the age at which they received their last dose)
The decision whether a reinforcing vaccine +/- human tetanus immunoglubin is required is based on an assessment of the wound, and knowledge of the tetanus vaccination status of the patient who suffered the tetanus - prone wound. This is summarised below. For up to date details then consult the Green Book (2).
Note:
- patients who are immunosuppressed may not be adequately protected against tetanus despite being fully immunised. The management should be similar to an incompletely immunised patient
Reference:
- Update on immunisation issues (August 2002). PL/CMO/2002/4,PL/CNO/2002/4,PL/CPHO/2002/2
- Department of Health (DH). Immunisation against infectious disease. 'The Green Book' 2019 updated edition
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page