Cancer and the immune system
Cancer and the immune system
- the basic role of our immune system is to protect human beings against foreign pathogens and also infections
- immune responses consist of two types:
- humoral immunity and cellular immunity, which are mediated by B and T lymphocytes as well as their products
- humoral immunity can neutralize and eradicate outside microbes and toxins via antibodies produced by B cells
- cellular immunity responds more quickly to eradicate intracellular microbes through recognition of antigens, activation of antigen presenting cells (APCs), activation and proliferation of T cells.
- humoral immunity and cellular immunity, which are mediated by B and T lymphocytes as well as their products
- immune responses consist of two types:
Both innate and adaptive immune systems play important roles in anticancer immune response
- innate immune cells can release signals which are essential to stimulate responses from both T cells and B cells
- adaptive immune system is mainly consists of B cells, CD8+ cytotoxic T cells as well as CD4+ helper T cells
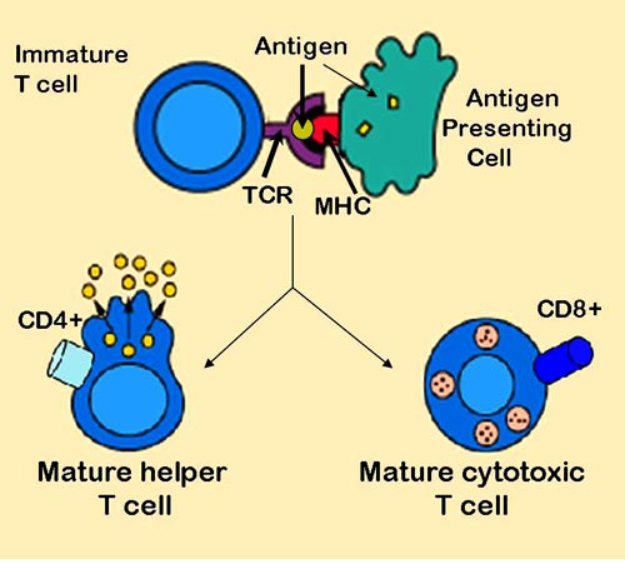
- APCs perform a bridge between the innate and the adaptive immune system by recognizing foreign antigens and presenting to the naive T cells
- after activation of toll-like receptors on dendritic cells (DCs), factors on the DC surface essential to antigen presentation are increased - cytokines that facilitate the adaptive immune response are promoted
- after activation of toll-like receptors on dendritic cells (DCs), factors on the DC surface essential to antigen presentation are increased - cytokines that facilitate the adaptive immune response are promoted
- Antigen presentation stimulates T cells to become either "cytotoxic" CD8+ cells or "helper" CD4+ cells (1)
- APCs perform a bridge between the innate and the adaptive immune system by recognizing foreign antigens and presenting to the naive T cells
- CD8+ cytotoxic T lymphocytes (CTLs) are fundamental in the immune response fighting cancer
- tumour-infiltrating lymphocytes (TILs) contain an abundant level of CTLs capable of invading malignant cells
- tumour antigen recognition
- necessary prerequisite for the effective anti-tumour immune response
- presentation mediated by direct presentation which cancer cells drain in the lymph node or via cross-presentation by pAPC
- professional antigen presenting cells (pAPCs) are immune cells that specialize in presenting an antigen to a T-cell
- main types of pAPCs are dendritic cells (DC), macrophages, and B cells
- pAPC takes up an antigen, processes it, and returns part of it to its surface, along with a class II major histocompatibility complex (MHC)
- the T-cell is activated when it interacts with the formed complex
- cross priming of naive CD8+ T cells by pAPC invokes a program leading to tumour specific CTLs proliferating and trafficking to the tumour sites where they will finally attack cancer cells
- CTLs can attack tumour cells via perforin, granzymes and also ligands of the tumour necrosis factor (TNF) superfamily
- anti-tumour effect can also be achieved by secreting Interferon gamma and TNF-alpha from activated CD8+ T cells
- naive CD4+ T cells could be activated and differentiated into distinct T cell subsets
- Th1, Th2, Tregs, Th9, Th17, Th22 and also follicular helper T cells once they encounter antigens and also adequate co-stimulation signals
- Th1 subset of CD4+ T cells play crucial antitumour roles by coordinating cell mediated immunity against cancer
- enhance CD8+ T cells expansion, priming and infiltration into the tumour site
- activate inflammatory cells, such as macrophages, NK cells, granulocytes and eosinophils in around the tumour
- can kill MHC-II+ tumour cells by releasing perforin and granzyme, and also by TNF-related apoptosis inducing ligand receptor and Fas/Fas ligand pathways
- NK cells can destroy cancer cells directly via:
- secretion of TNF-alpha, perforin, cytoplasmic granules and granzymes, expression of death receptor-mediated apoptosis, and expression of CD16 which leads to antibody dependent cellular cytotoxicity (ADCC)
- NK cells have been able to have antitumour activity as well indirectly by chemokines, cytokines and growth factors production
- macrophages can be characterized as pro-inflammatory M1 or anti-inflammatory M2 macrophages:
- M1 macrophages secrete pro-inflammatory cytokines boost antitumour immunity
- M2 macrophages produce anti-inflammatory cytokines which would promote tumourogenesis
Reference:
- Brooks M, Olsson-Brown A. Summary on Immunotherapy for Palliative Care Teams
- Haanan J et al. Management of toxicities from immunotherapy: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up, Annals of Oncology 2017; 28 (Supplement 4)
- Zhang H, Jibei C. Current status and future directions of cancer immunotherapy. Journal of Cancer 2018; 9(10): 1773-1781.
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page