When contraception can be stopped
Menopause is usually a clinical diagnosis made retrospectively after 1 year of amenorrhoea (1)
- most women do not require measurement of their serum hormone levels to make the diagnosis (1)
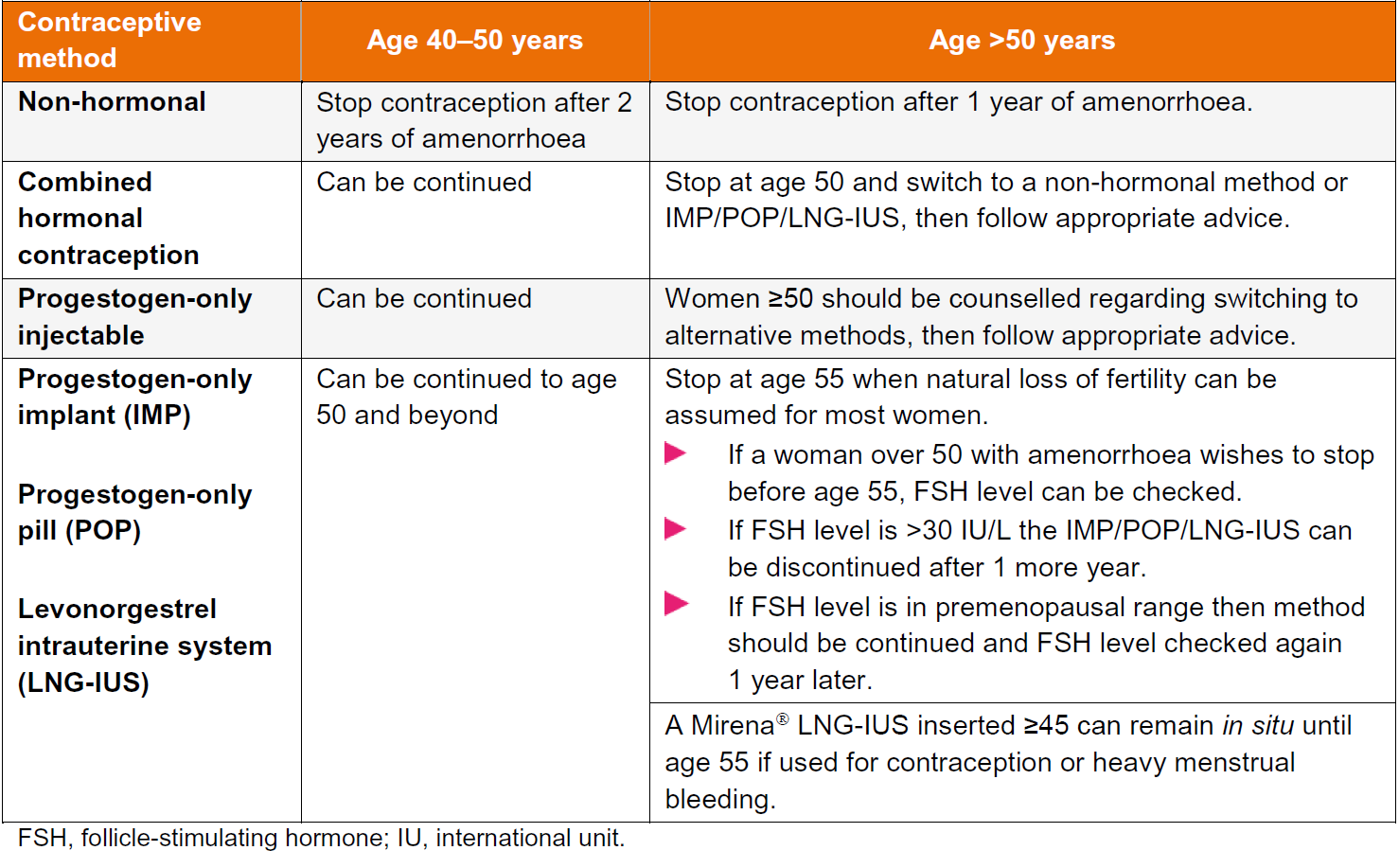
If not using hormonal contraception then:
- if under 50 years can stop contraception after two years amenorrhoea (1,2,3,4)
If using contraception:
- if needed, women over 50 using progestogen-only contraception, including DMPA, can have serum follicle-stimulating hormone (FSH) measurements undertaken to check menopausal status
- the post-menopause is characterised by low levels of serum estradiol and raised levels of FSH and LH. As a general guide, a serum FSH level >30 IU/L indicates a degree of ovarian insufficiency, but not necessarily sterility (4)
- during perimenopause, isolated serum estradiol, FSH and LH levels can be misleading and should not be used as a basis for providing advice about stopping contraception; ovulation may still occur with risk of pregnancy, particularly in young women with a diagnosis of premature ovarian insufficiency.For this reason, the FSRH suggests restricting measurement of serum FSH for advice about stopping contraception to women over 50 using POC (non-injectable progestogen-only contraception) who are amenorrhoeic (4)
- women using CHC (combined hormonal contraception) or HRT (hormone replacement therapy) have suppressed levels of estradiol and gonadotrophins (FSH/LH)
- measuring these hormones does not give accurate information on which to base advice regarding menopausal status and when to stop contraception
- if using COC - can be prescribed in low-risk women until aged 50 years
- at aged 50 years switch to an alternative method of contraception. Subsequently follow advice on stopping contraception as per method used
- in general, all women can cease contraception at age 55 as spontaneous conception after this age is exceptionally rare even in women still experiencing menstrual bleeding
- if a woman aged 55 or over does not wish to stop a particular method, consideration can be given to continuation providing the benefits and risks for her as an individual have been assessed and discussed with her (4)
- IUC should not be left in situ indefinitely after it is no longer required as it could become a focus of infection.
Recommendations regarding stopping contraception
Notes:
- after counselling (about declining fertility, risks associated with insertion, and contraceptive efficacy), women who have a Cu-IUD containing >=300 mm2 copper, inserted at or over the age of 40 years, can retain the device until the menopause or until contraception is no longer required
- women who continue to use their IUD until contraception is no longer required should be advised to return to have the device removed
- if a woman is using DMPA and has elevated FSH levels, HCPs can be confident that the increased levels are due to perimenopause
- DMPA can suppress FSH to some extent which means a woman using DMPA could be menopausal yet show no increase in FSH levels. The optimum time to measure FSH levels in a woman using DMPA is just before a repeat DMPA is administered
- the Mirena can remain in situ for contraception until menopause if inserted at or after the age of 45
Reference:
- Prescribers’ Journal 2000;40 (2):121-129.
- Pulse September 17th 2005: 62-4
- FSRH (2010). Contraception for Women Aged Over 40 Years.
- FSRH (2019). Contraception for Women Aged Over 40 Years.
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page