Starting or switching from an MAOI
Summary guidance regarding switching to or from an MAOI states (1):
- care is required when switching between antidepressants.
- when switching between monoamine-oxidase inhibitor (MAOI) or moclobemide (a reversible inhibitor of monoamine-oxidase type A- RIMA) and other antidepressants, the first antidepressant agent should be withdrawn gradually and discontinued before starting the second antidepressant
- for switches that involve a MAOI, a washout period is always advised
- patients should be assessed on an individual basis to determine how quickly the switch can be made by assessing history of discontinuation reactions, concurrent medication and severity of depression
- the potential for medication errors should be considered
MAOI discontinuation syndrome (2):
- reactions to MAOI discontinuation, particularly those reported with tranylcypromine, tend to be more severe than with other antidepressants (2)
- features may include:
- (i) a worsening of depressive symptoms, exceeding the severity of the state that originally led to treatment
- (ii) an acute confusional state with disorientation, paranoid delusions and hallucinations
- (iii) anxiety symptoms, including hyperacusis and depersonalisation
Non-reversible MAOIs, such as phenelzine, combined antidepressants and lithium augmentation of antidepressants should normally be prescribed only by specialist mental health professionals (3)
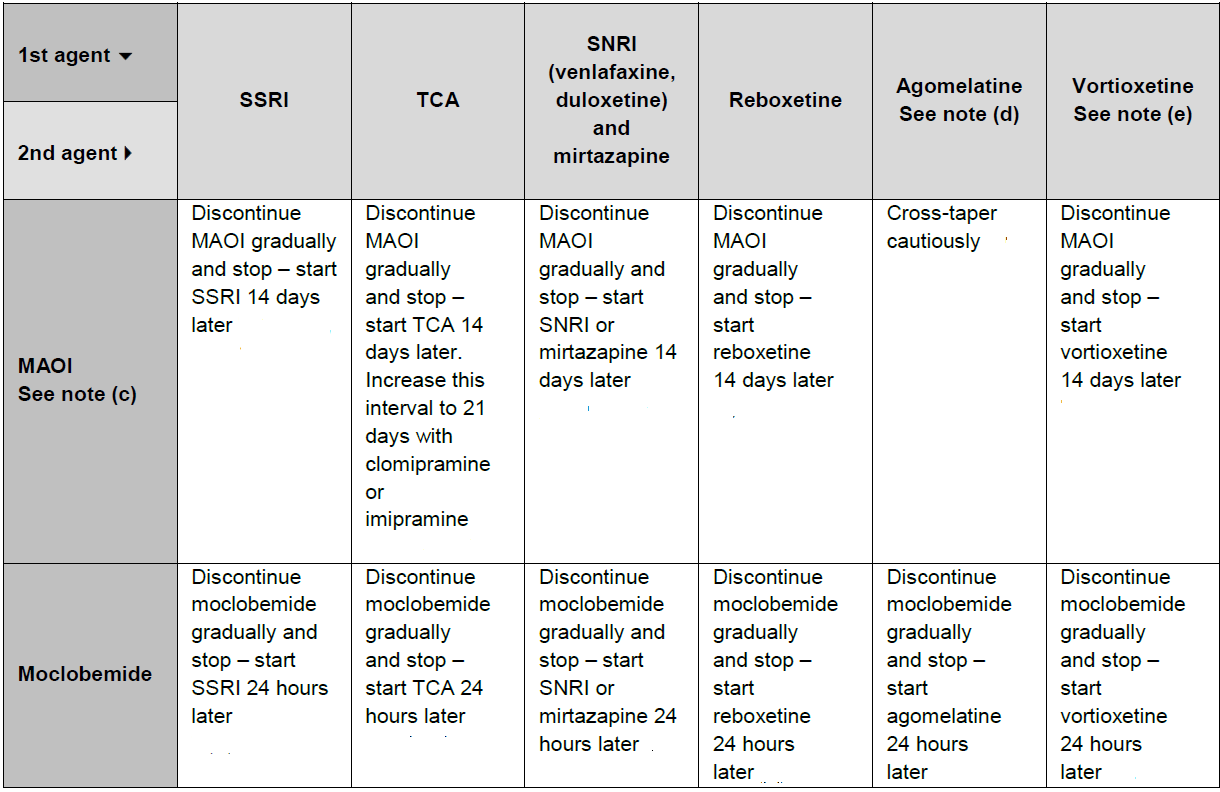
- when switching from a non-reversible MAOI: a 2-week washout period is required (do not routinely prescribe other antidepressants during this period) (3)
- 3 weeks with clomipramine or imipramine (4). Only experienced psychiatrists should use selected tricyclics in conjunction with MAOIs as this is potentially fatal. There is no evidence that the combination is more effective than when either constituent is used alone
- combination of tranylcypromine with clomipramine is particularly dangerous (4)
Reports of hyperactivity, hypertonicity, hyperpyrexia, coma and death have been associated with the use of tranylcypromine in combination with tricyclic antidepressants; Tetracyclic antidepressants should also be avoided. The use of clomipramine in patients already on tranylcypromine may be particularly hazardous (4)
Switches between selective serotonin reuptake inhibitors (SSRIs), tricyclics (TCA) and serotonin-noradrenaline reuptake inhibitor (SNRI) antidepressants and either a monoamine-oxidase inhibitor (MAOI) or moclobemide (a reversible inhibitor of monoamine-oxidase type A - RIMA) require a washout period between stopping one agent and starting another to avoid the potential risk of serotonin syndrome
- the first antidepressant should be gradually withdrawn over several weeks and the second antidepressant started after a suitable washout period
Switching to an MAOI or moclobemide:
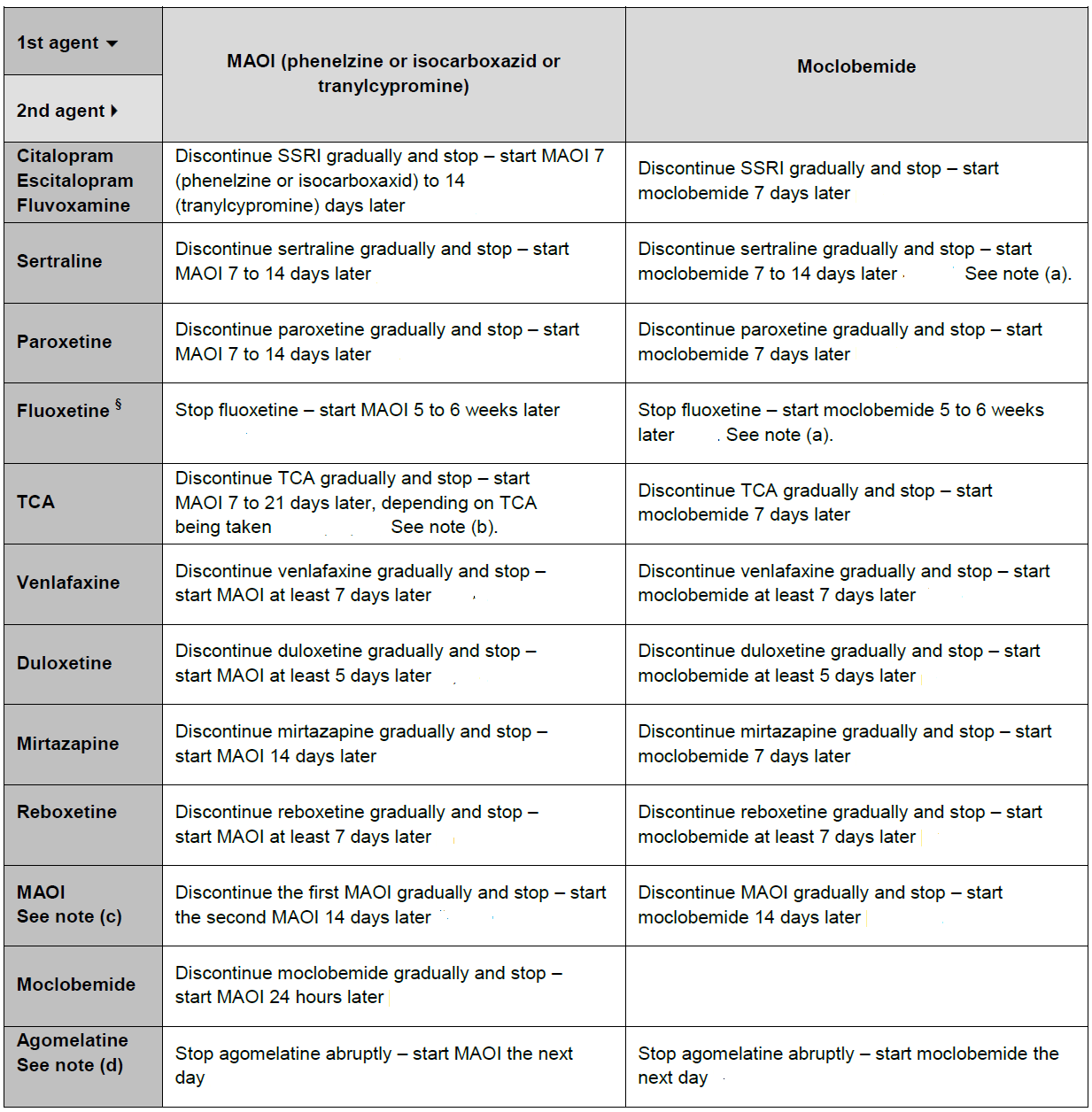
a. SSRI to moclobemide
- when switching from an SSRI to moclobemide, the Summary of Product Characteristics (SmPC) for citalopram, fluvoxamine, sertraline and paroxetine recommend a washout period of seven days before starting moclobemide whilst other sources suggest a longer washout period of 13 days for sertraline due to its half-life
- fluoxetine has a longer half-life than the other SSRIs, a washout period of five to six weeks is recommended before initiating moclobemide
b. TCA to MAOI
- when switching from a TCA to a MAOI, general advice is to allow at least a seven day washout period before starting treatment with low-dose MAOI
- however, the SmPC for phenelzine tablets advises a 14 day washout period after stopping a TCA - should be extended to 21 days if the TCA is clomipramine or imipramine as these are more potent inhibitors of serotonin reuptake and the risk of serotonin syndrome will consequently be increased
- BNF suggests a seven to 14 day washout period, extended to 21 days if clomipramine or imipramine have been taken
- switches involving tranylcypromine, phenelzine, clomipramine or imipramine, are at greater risk of adverse reactions due to their potent effects on serotonin reuptake
- switching between any of these agents should be done with extreme caution
c. MAOI withdrawal
- withdrawal of an MAOI should be over four weeks or longer if symptoms of withdrawal emerge (6 months in patients who have been on long-term maintenance treatment)
- features of MAOI withdrawal include nausea, vomiting, malaise, nightmares, agitation, irritability, movement disorders, insomnia, slowed speech and convulsions. Symptoms usually respond to initiation of low-dose MAOI therapy followed by cautious downward titration and discontinuation
d. Agomelatine
- agomelatine is an antidepressant agent with selective agonist action at melatonin receptors and selective antagonist action at serotonin 5HT-2C receptors
- does not affect uptake of serotonin, noradrenaline or dopamine
- abrupt withdrawal of agomelatine has not been associated with discontinuation symptoms - means that no dose tapering is necessary when stopping treatment
- no significant problems have been reported when agomelatine is taken with most other antidepressants so patients can be switched to and from this with negligible risk
- when switching from a MAOI to agomelatine, agomelatine can be started whilst gradually withdrawing the first antidepressant.
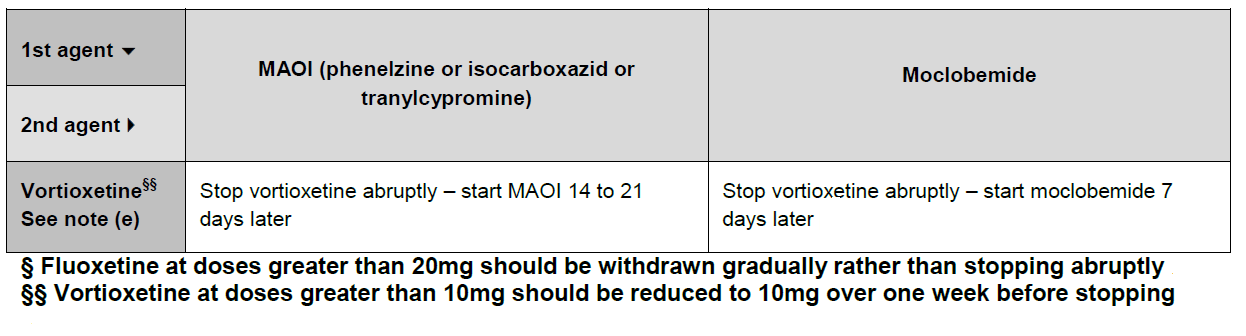
e. Vortioxetine
- vortioxetine is a relatively new antidepressant and there is limited experience when switching, therefore extra caution is required
- when switching to another antidepressant, doses above 10mg should be reduced to 10mg over a period of 7 days before stopping and starting the new antidepressant
- when switching from vortioxetine to a MAOI, the manufacturer recommends a 14 day interval [16]. Another source suggests a gap of 21 days [2].
Switching from an MAOI or moclobemide to SSRI, TCA or related antidepressants
Notes:
- symptoms of antidepressant discontinuation syndrome are likely when a drug is stopped abruptly after regular administration for six weeks or more
- most antidepressants should be withdrawn by reducing the dose gradually over a minimum of four weeks, using patient's symptoms as a guide to the speed of withdrawal
- fluoxetine and vortioxetine are the exceptions. Because of their long half-lives, vortioxetine can be stopped abruptly as can fluoxetine at a dose of 20mg daily (at higher doses, incremental withdrawal is required with fluoxetine)
- most antidepressants should be withdrawn by reducing the dose gradually over a minimum of four weeks, using patient's symptoms as a guide to the speed of withdrawal
Reference:
- NHS Specialist Pharmacy Service (April 2019). How do you switch between monoamine oxidase inhibitors and SSRI, tricyclic or related antidepressants?
- Anderson IM et al (2000). Evidence-based guidelines for treating depressive disorders with antidepressants: a revision of the 1993 British Association for Psychopharmacology guidelines. J Psychopharmacol; 14: 3-20.
- NICE (June 2019). Antidepressant treatment in adults.
- Dorset Medicines Advisory Group. Shared Care Guidelines for the use of monoamine oxidase inhibitors (MAOIs) - Phenelzine and Isocarboxazid (Accessed 18/9/2019)
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page