Clinical features
The clinical features of this condition are dependent on the organism involved.
Presentation of patients with symptoms varies according to the incubation period of the parasite. (1)
- falciparum infection - most present within the first month or months after exposure and all most all present within 6 months
- vivax and ovale infection - most present later than 6 months after exposure or may be years after exposure
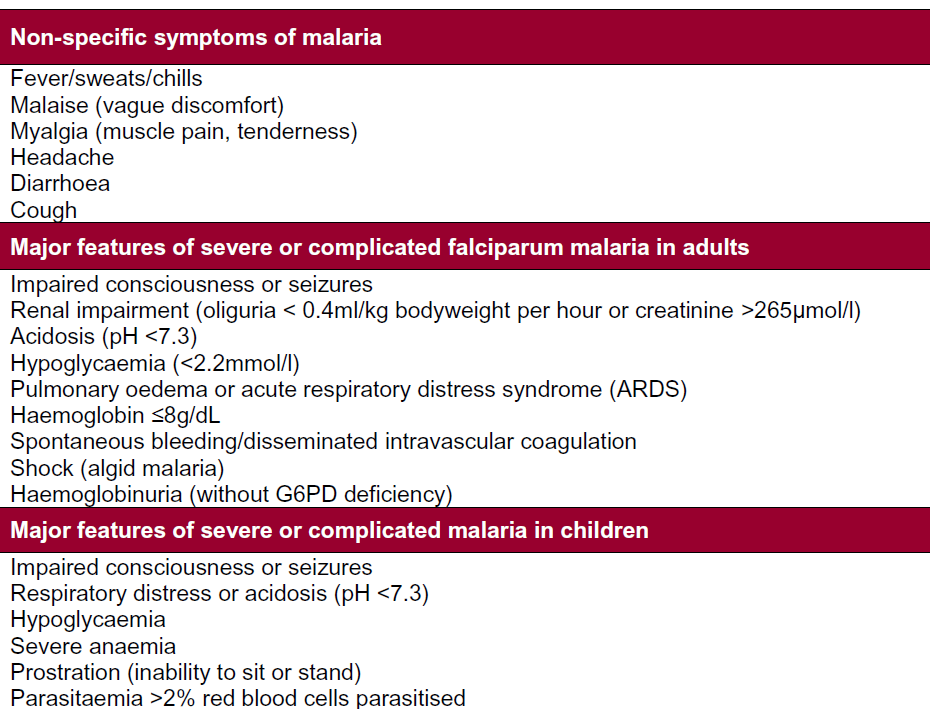
"Uncomplicated malaria" may present with a prodrome of non specific symptoms:
- malaise
- headache
- muscular ache
- diarrhoea
- dry cough
Following the prodrome the patient develops paroxysms lasting 8 to 12 hours, which consists of 3 stages:
- a cold stage - sudden coldness, followed by a severe rigor for up to an hour
- a hot stage - a high temperature, vomiting, flushing and
- finally a sweating stage - sweating, return to normal temperature, tiredness
Although rarely seen these paroxysms usually occur
- every 48 hours with "tertian" infection (P. falciparum, P. vivax, and P. ovale)
- every 72 hours with "quartan" infections (P. malariae)
Children are more likely to have non specific symptoms like irritability, lethargy and gastrointestinal symptoms (diarrhoea and vomiting) and the disease may worsen over a short period of time.
"Severe or complicated malaria" which is almost always caused by P falciparum (on rare occasions by P. vivax) presents with the following signs or symptoms:
- impaired consciousness or seizures ¢ renal impairment (oliguria < 0.4 ml/kg bodyweight per hour or creatinine > 265mmol/l)
- acidosis (pH < 7.3)
- hypoglycaemia (<2.2 mmol/l)
- pulmonary oedema or acute respiratory distress syndrome (ARDS)
- haemoglobin <=8 g/dL
- spontaneous bleeding/disseminated intravascular coagulation
- shock (algid malaria e BP < 90/60 mmHg)
- haemoglobinuria (without G6PD deficiency
PHE have summarised clinical features as (2):
Reference:
- Lalloo DG, Shingadia D, Bell DJ, et al. UK malaria treatment guidelines 2016. J Infect. 2016 Jun;72(6):635-49.
- UK Health Security Agency. Malaria prevention guidelines for travellers from the UK. Published July 2014, last updated April 2025
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.