Surgical treatment
Surgery is only indicated in a minority of patients with diverticular disease. In these, recurrent acute diverticulitis is usually the indication for simple removal of the affected segment of bowel. A provisional transverse colostomy may be required before resection if there are acute complications, e.g. inflammation or bowel obstruction. Formal resection is carried out as soon as inflammation has subsided, typically after 2-3 weeks.
NICE have suggested surgical management in diverticular disease (1):
Management of abscesses
For people presenting in secondary care with complicated acute diverticulitis and suspected diverticular abscess, assess and manage in consideration of possible sepsis.
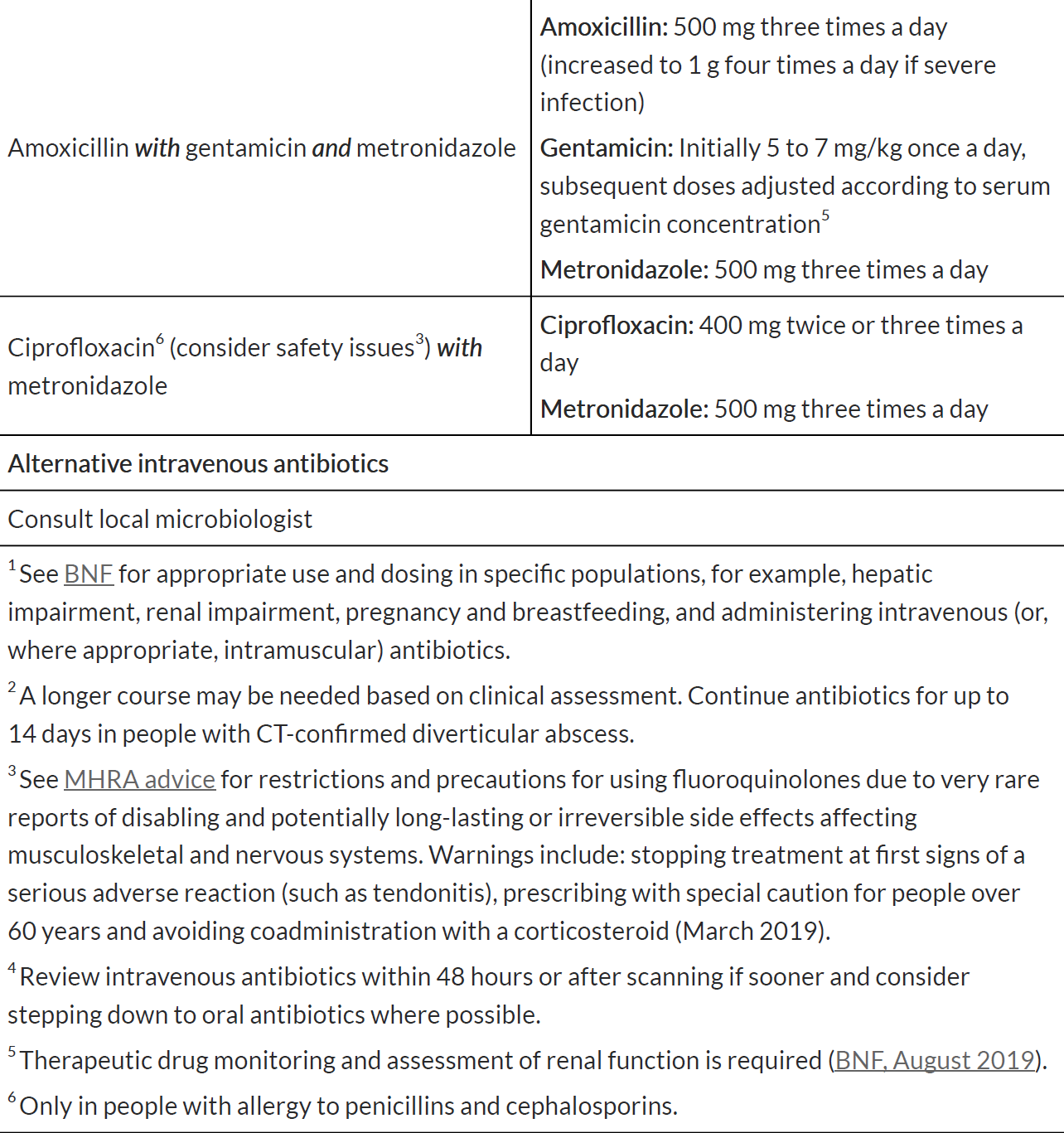
Offer intravenous antibiotics to people with acute diverticulitis and suspected diverticular abscess.
When prescribing an antibiotic for diverticular abscess, follow the advice in table below.
Offer a contrast CT scan to people with acute diverticulitis and suspected diverticular abscess. If contrast CT is contraindicated, perform one of the
following:
- a non-contrast CT or
- an MRI or
- an ultrasound scan, depending on local expertise
Review intravenous antibiotics within 48 hours or after scanning if sooner and consider stepping down to oral antibiotics where possible.
Use the scan results to guide treatment based on the size and location of the abscess.
If a person does not have confirmed diverticular abscess, review their need for antibiotics.
Consider either percutaneous drainage (if anatomically feasible) or surgery for abscesses greater than 3 cm.
Send samples of pus from the abscess (if it has been drained) to the microbiology laboratory to enable antibiotic treatment to be tailored to sensitivities.
For abscesses less than 3 cm switch to oral antibiotics where possible.
In people with a CT-confirmed diverticular abscess, if the condition does not improve clinically or there is deterioration, consider re-imaging to inform the
management strategy.
Management of bowel perforations:
Offer either laparoscopic lavage or resectional surgery to people with diverticular perforation with generalised peritonitis after
discussing the risks and benefits of the 2 options with them. If faecal peritonitis is identified intraoperatively, proceed to resectional surgery
Anastomosis and bowel resection for people with complicated acute diverticulitis (elective and emergency surgery)
Offer people with complicated acute diverticulitis who are having surgery (either elective or emergency):
- primary anastomosis (join in the bowel) with or without diverting stoma or
- Hartmann's procedure (resection of the bowel with an end stoma)
Take into account the person's age, any other conditions they have and how well they can carry out everyday activities (WHO performance status).
In people undergoing bowel resection, consider resecting back to the compliant bowel (that is, bowel that is soft, unthickened and unaffected by inflammation).
Notes:
Reference:
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page