Management of food allergy
Primary prevention of food allergy:
- no special diet during pregnancy or lactation
- advised to have exclusive breast feeding for 6 months (but at least for 4 months). If supplement is required then conventional cow's milk formula is recommended
- avoid solid foods for at least 4 months (preferabley 6 months)
- if high-risk infants (one parent or sibling with allergic disease)
- if a supplement is required then an extensively hydrolysed protein formula is recommended for the infant until 4 months of age (1). If the infant is aged over 4 months and has no signs of allergic disease, then can be nourished like normal infants
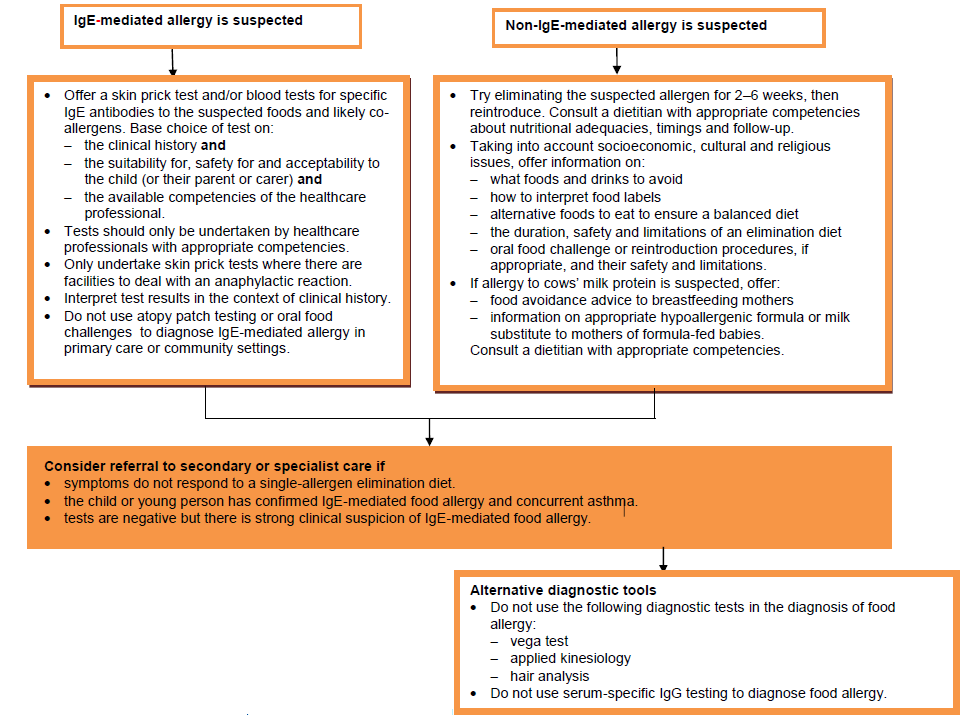
Referral to secondary or specialist care
Based on the allergy-focused clinical history, consider referral to secondary or specialist care in any of the following circumstances.
- the child or young person has:
- faltering growth in combination with one or more of the gastrointestinal symptoms
IgE-mediated | non-IgE-mediated |
Angioedema of the lips, tongue and palate | Gastro-oesophageal reflux disease |
Oral pruritus | Loose or frequent stools |
Nausea | Blood and/or mucus in stools |
Colicky abdominal pain | Abdominal pain |
Vomiting | Infantile colic |
Diarrhoea | Food refusal or aversion |
Constipation | |
Perianal redness | |
Pallor and tiredness | |
Faltering growth in conjunction with at least one or more gastrointestinal symptoms above (with or without significant atopic eczema) |
- not responded to a single-allergen elimination diet
- had one or more acute systemic reactions
- had one or more severe delayed reactions
- confirmed IgE-mediated food allergy and concurrent asthma
- significant atopic eczema where multiple or cross-reactive food allergies are suspected by the parent or carer.
- There is:
- persisting parental suspicion of food allergy (especially in children or young people with difficult or perplexing symptoms) despite a lack of supporting history strong clinical suspicion of IgE-mediated food allergy but allergy test results are negative
- clinical suspicion of multiple food allergies
NICE state (3):
Treatment of established allergy:
- removal of causal allergen from both the infant and maternal diets (if breast feeding)
- for management of cow's milk protein allergy then see linked item
Provision of an Epipen
This has been recommended if any child falls into one of the following categories:
- previous respiratory or cardiovascular reaction
- reaction to trace amount of protein
- co-existant asthma (as a risk factor for severe reactions)
- allergy to peanuts or tree nuts (as subsequent reactions may be more severe)
Notes:
- soya is not recommended before 6 months of age due to it containing isoflavones, which may exert a weak oestrogenic effect. There is also a risk of cross-reactivity: up to 14% of those with IgE-mediated cow’s milk allergy also react to soya and up to 60% of those with non-IgE-mediated cow’s milk allergy
- rice milk is not recommended in those aged <4.5 years due to the arsenic content; and there is cross-reaction between mammalian milks
- goat’s milk and products are not suitable for infants with cow’s milk allergy
- most children lose their sensitivity to allergenic foods within the first 3-5 years of life
- systematic reviews have been undertaken concerning the use of soy formula and formulas containing hydrolysed protein for the prevention of food intolerance:
- feeding with a soy formula cannot be recommended for prevention of allergy or food intolerance in infants at high risk of allergy or food intolerance (4)
- further research may be warranted to determine the role of soy formulas for prevention of allergy or food intolerance in infants unable to be breast fed with a strong family history of allergy or cow's milk protein intolerance
- no evidence to support feeding with a hydrolysed formula for the prevention of allergy compared to exclusive breast feeding. In high risk infants who are unable to be completely breast fed, there is limited evidence that prolonged feeding with a hydrolysed formula compared to a cow's milk formula reduces infant and childhood allergy and infant cow's milk allergy (5)
- feeding with a soy formula cannot be recommended for prevention of allergy or food intolerance in infants at high risk of allergy or food intolerance (4)
Reference:
- Pulse (March 26th 2005): 50-57.
- Sicherer SH.Food allergy. The Lancet 2002; 360(9334):701-710
- NICE. Food allergy in children and young people: diagnosis and assessment of food allergy in children and young people in primary care and community settings. CG 116. 2011
- Osborn DA, Sinn J. Soy formula for prevention of allergy and food intolerance in infants. Cochrane Database Syst Rev. 2006 Oct 18;(4):CD003741.
- Osborn DA, Sinn J. Formulas containing hydrolysed protein for prevention of allergy and food intolerance in infants. Cochrane Database Syst Rev. 2006 Oct 18;(4):CD003664.
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page