ALT in diabetes
- liver function tests (LFTs) generally include:
- serum aminotransferases, alkaline phosphatase, bilirubin, albumin (measures of clotting function such as prothrombin time may also be included in a liver function test profile)
- aminotransferases (alanine aminotransferase (ALT) and aspartate aminotransferase (AST)) measure the concentration of intracellular hepatic enzymes that have leaked into the circulation - these serve as a marker of hepatocyte injury
- alkaline phosphatase (AP), gamma-glutamyl transpeptidase (GGT), and bilirubin act as markers of biliary function and cholestasis
- albumin and prothrombin reflect liver synthetic function
- non-alcoholic fatty liver disease (NAFLD) includes a wide spectrum of liver pathology, ranging from fatty liver alone to the more severe nonalcoholic steatohepatitis (1)
- NAFLD is the most common cause of chronically elevated LFTs in the United States in both diabetic and nondiabetic individuals
- with respect to patients with NAFLD, 60-95% are obese, 28-55% have type 2 diabetes, and 20-92% have hyperlipidemia (2)
- if NAFLD develops in people who are not heavy drinkers then the condition generally has a benign clinical course (3,4)
- NAFLD is a cause of hepatic inflammation histologically resembling that of alcohol-induced liver disease but usually slowly progressive and of low-grade severity. ..However, the disorder may ultimately result in cirrhosis (4)
- there is evidence of associations between NAFLD and obesity, dyslipidaemia and insulin resistance (4,5)
- NAFLD generally results in an asymptomatic elevation of liver enzyme levels (6), including ALT and AST - ALT is primarily found in the liver whereas AST is also found in other tissues and is a less specific marker of liver integrity
- in the setting of marker-negative elevated LFTs, the most likely histological diagnosis is fatty metamorphosis of the liver with occasional associated fibrosis (6)
- significant iron accumulation is not seen in NAFLD (7)
- NAFLD is the most common cause of chronically elevated LFTs in the United States in both diabetic and nondiabetic individuals
- raised levels of ALT is a also a risk factor for the development type 2 diabetes and indicates a potential role of increased hepatic gluconeogenesis and/or inflammation in the pathogenesis of type 2 diabetes (2)
- prospective studies found that levels of ALT predicted incident type 2 diabetes - this was independent of the classical risk factors or changes in obesity
- prospective studies found that levels of ALT predicted incident type 2 diabetes - this was independent of the classical risk factors or changes in obesity
- hepatitis C virus (HCV) is a known independent predictor of type 2 diabetes (2)
- HCV is known to have a higher prevalence within diabetic patients (2)
- with respect to abnormal liver function tests in type 2 diabetes (2)
- BMI > 25 kg/m2 and poor diabetic control fasting blood glucose were the most significant clinical variables associated with elevated ALT and GGT
- raised levels of ALT were also associated with onset of diabetes within the past 4 years, mature onset of diabetes (35-51 years), and use of diet or sulphonylurea medication
- with respect to abnormal liver function tests in type 1 diabetes (8)
- these were associated with diabetic complications such as retinopathy and neuropathy, independently of alcohol consumption, BMI and glycaemic control. There was also an association between raised GGT and limited joint mobility
- these were associated with diabetic complications such as retinopathy and neuropathy, independently of alcohol consumption, BMI and glycaemic control. There was also an association between raised GGT and limited joint mobility
- in conclusion (2):
- individuals with type 2 diabetes have a higher incidence of LFT abnormalities than individuals who do not have diabetes
- the most commonly abnormal LFT is a raised ALT
- any diabetic patient found to have a mild chronic elevation of ALT should have screening for treatable causes of chronic liver disease - this screening should include hepatitis B, hepatitis C, and hemochromatosis, which are found with increased incidence in type 2 diabetes
- if there are no other causes of raised LFTS such as medications, alcohol, autoimmunity, metabolic etiology, or hereditary causes, and for those who have no evidence of more serious liver disease (e.g. raised alkaline phosphatase, raised bilirubin, increased prothrombin time or decreases in albumin) then it has been suggested that further diagnostic workup is probably not required (2). Other sources would consider further investigation such as an ultrasound scan if ALT persists > 80 IU/L and specialist referral if ALT > 120 IU/L or persistently ALT > 80 IU/L after three months (10,11)
- raised levels of ALT within three times the upper limit of normal is not a contraindication for starting any oral antidiabetic or lipid modifying therapy (2). If improved glycaemic control is achieved then antidiabetic agents have generally been shown to decrease ALT levels
- individuals with type 2 diabetes have a higher incidence of LFT abnormalities than individuals who do not have diabetes
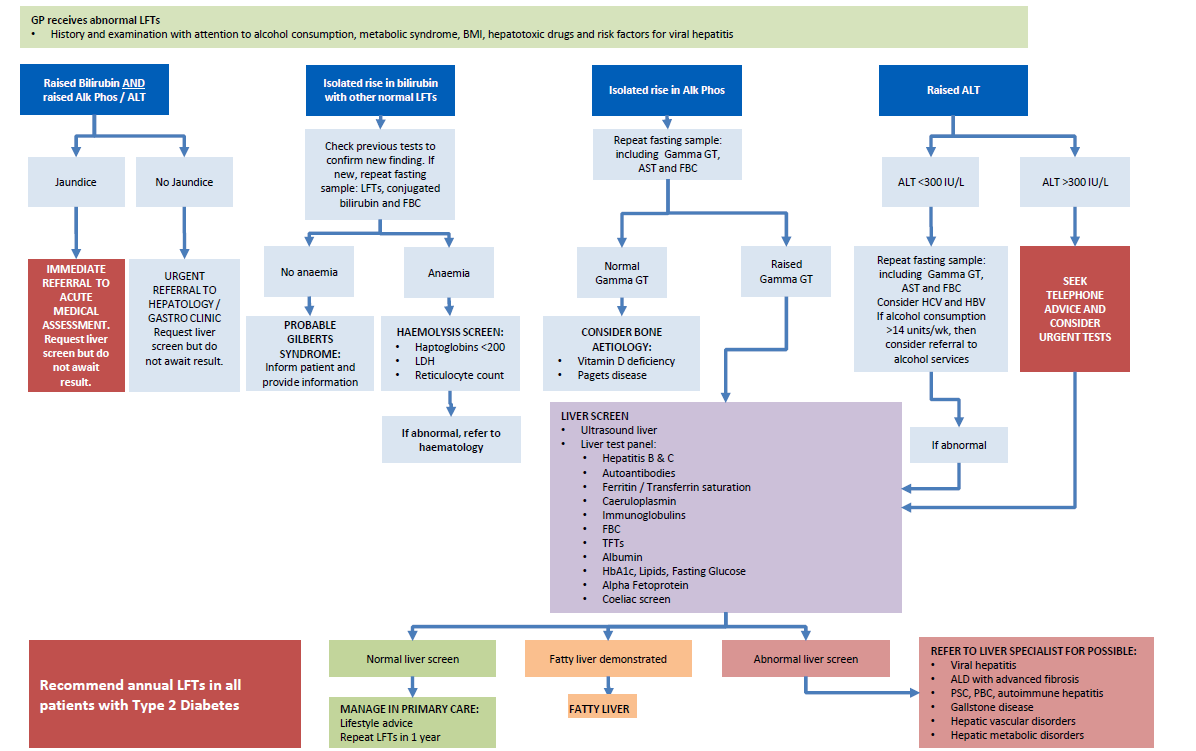
A suggested schemata for investigating abnormal LFTs in type 2 diabetes is presented below (12) - note that if hepatic or biliary malignancy is suspected then urgent secondary care referral is indicated rather than detailed investigation in primary care.
Reference:
- Angulo P. Nonalcoholic fatty liver disease. N Engl J Med 2002;346: 1221-31.
- Harris EH.Elevated Liver Function Tests in Type 2 Diabetes.Clinical Diabetes 2005; 23:115-119.
- Matteoni CA, Younossi ZM, Gramlich T, Boparai N, Liu YC, McCullough AJ. Nonalcoholic fatty liver disease: a spectrum of clinical and pathological severity. Gastroenterology 1999;116: 1413-9.
- Powell EE, Cooksley WG, Hanson R, Searle J, Halliday JW, Powell LW. The natural history of nonalcoholic steatohepatitis. a follow-up study of forty-two patients for up to 21 years. Hepatology 1990;11: 74-80.
- Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology 2003;37: 917-23.
- Daniel S, Ben Menachem T, Vasudevan G, Ma CK, Blumenkehl M. Prospective evaluation of unexplained chronic liver transaminase abnormalities in asymptomatic and symptomatic patients. Am J Gastroenterol 1999;94: 3010-4.
- Hepatology. 1999 Oct;30(4):847-50.
- Arkkila PE, Koskinen PJ, Kantola IM, Ronnemaa T, Seppanen E, Viikari JS. Diabetic complications are associated with liver enzyme activities in people with type 1 diabetes. Diabetes Res Clin Pract 2001;52: 113-8
- Schindhelm RK et al. Liver alanine aminotransferase, insulin resistance and endothelial dysfunction in normotriglyceridaemic subjects with type 2 diabetes mellitus. European Journal of Clinical Investigation 2005; 35(6): 369.
- Pulse (2004); 64 (3): 34-6.
- Pratt DS, Kaplan MM. Evaluation of abnormal liver-enzyme results in asymptomatic patients. NEJM 2000;342:1266-71.
- The North West London Health and Care Partnership. North West London Diabetes Guidelines (Accessed 23/9/2020).
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page