Ramadan - implications for patients with type 2 diabetes
Ramadan fasting (or sawm) is one of the Five Pillars of Islam, considered by believers to be the foundation of Muslim life. Fasting occurs in the ninth month of the Islamic calendar (Hijra). The Islamic calendar is lunar based and has only 354 days. It therefore occurs 11 days earlier each year.
Ramadan has great religious and cultural importance for Muslims. Healthcare professionals need to understand the impact this has on people with diabetes.
In regions at the extremes of latitude, the amount of daylight hours(the number of daily fasting hours) can be up to 20 hours in summer and 10 hours in winter.
Fasting during Ramadan (1,2):
- healthy adult Muslims fast from sunrise to sunset during Ramadan. A light meal is eaten before sunrise (Sohour) before the start of the fasting period. After the fasting period a large meal, often with extra savoury and sweet foods (Iftar) is eaten
- fasting entails abstinence from food, liquid and oral medications
- fasting period occurs between sunrise (suhoor) and sunset (iftar)
- Ramadan lasts for 29–30 days
- in the UK, a fast lasts 10–21 hours, depending on the season in which Ramadan falls
- not everyone has to fast. An individual can be exempt if they have an illness whereby fasting is detrimental
- fasting entails abstinence from food, liquid and oral medications
- patients with diabetes who fast should eat a healthy, balanced diet at all other times
- patients with diabetes should avoid eating large amounts of food at the break of the fast. Instead, patients with diabetes should take two or three smaller meals in the non-fasting period (2)
- during Ramadan, the pre-dawn meal should be eaten as close to the start of the fast as possible. At this time, foods rich in complex carbohydrate are preferable as they are digested over a number of hours, whereas sugary foods are preferable at the break of fast (2)
- fasting is not recommended if the type 2 diabetic patient has significant kidney disease. Also heart failure, current infections, pregnancy and poorly controlled diaetes are contraindications to fasting (1)
Pre-Ramadan diabetes education (3,4):
- a pre-Ramadan diabetes education session is advised 1–2 months before the fasting period. The benefits of a structured diabetes education programme with a Ramadan focus include fewer hypoglycaemic episodes, weight loss and improved glycaemic control(3). There are six key areas that should be covered:
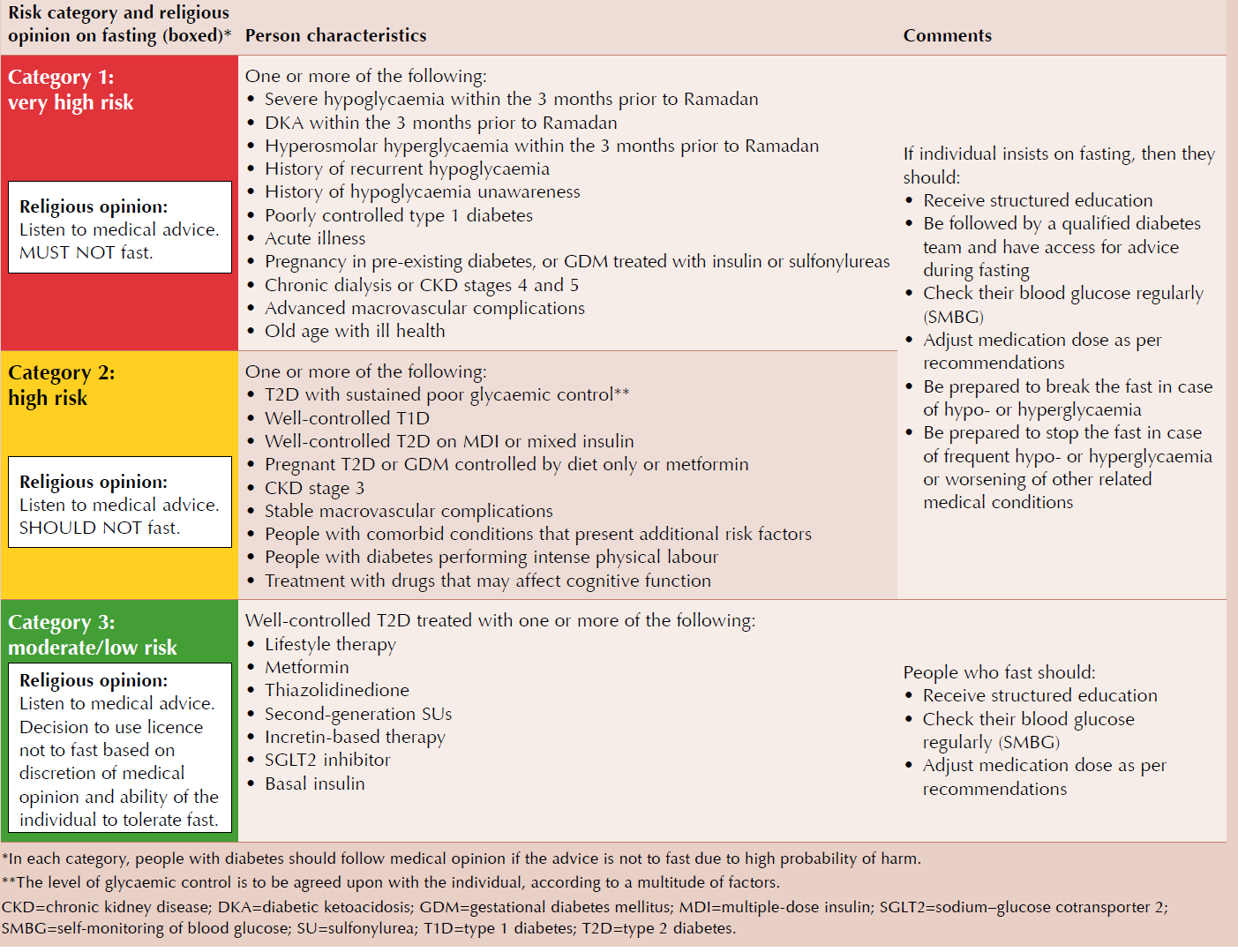
- Risk quantification. Individuals can be stratified into one of three risk categories identified by IDF-DAR(3). These are very high risk, high risk or moderate/low risk (see table over page)
- When to break the fast. A fast should be broken if: blood glucose levels are <3.9 or >16.7 mmol/L; there are symptoms of hypoglycaemia; or an acute illness occurs
- Exercise. Light-to-moderate exercise is advisable during Ramadan.
- Fluids and dietary advice. A Ramadan nutrition plan is recommended (see below)
- Blood glucose monitoring. It is advisable to check blood glucose levels several times a day. This does not constitute breaking the fast
- When to check blood glucose during Ramadan fasting
1. Pre-dawn meal (suhoor)
2. Morning
3. Midday
4. Mid-afternoon
5. Pre-sunset meal (iftar)
6. 2 hours after iftar
7. Any time when symptoms of hypo- or hyperglycaemia, or feeling unwell
- When to check blood glucose during Ramadan fasting
- Medication adjustment (see below)
Fluids and Dietary Advice (4):
- Key messages include:
- Low glycaemic index (GI), high fibre foods for slow energy release.
- Begin iftar with 1–2 dates to raise blood glucose levels and plenty of water to overcome dehydration.
- Avoid other sugary foods.
- Eat balanced meals:
- 45–50% carbohydrate,
- 20–30% protein and
- <35% fat
- Take suhoor as late as possible
- Maintain hydration with water and non-sweetened beverages overnight between iftar and suhoor
- Eat foods that induce satiety (i.e. with protein and fibre)
IDF-DAR (3) risk categories and recommendations for people with diabetes who fast during Ramadan
Medications Adjustment (4):
Metformin
- daily dose remains unchanged
- Immediate release:
- daily – take at iftar;
- twice daily – take at iftar and suhoor;
- three-times daily – morning dose at suhoor, combine afternoon and evening dose at iftar
- prolonged release: take at iftar
Sulfonylurea (SU)
- switch to newer SU (gliclazide, glimepiride) where possible; glibenclamide should be avoided
- once daily – take at iftar. Dose may be reduced in people with good glycaemic control
- twice daily – iftar dose remains unchanged. Suhoor dose should be reduced in people with good glycaemic control.
- for once-daily SU combination therapy, take at iftar and consider reducing the dose by 50%
- for twice-daily SU combination therapy, omit morning dose and take normal dose at iftar
- consider switching permanently to drugs withlow risk of hypoglycaemia (GLP-1 antagonists, SGLT-2 inhibitors) (8)
Prandial glucose regulators (glinides)
- three-times daily dosing may be reduced/redistributed to two doses taken with iftar and suhoor
- consider switching permanently to drugs withlow risk of hypoglycaemia (GLP-1 antagonists, SGLT-2 inhibitors) (8)
Thiazolidinediones
- no dose modifications.
- dose can be taken with iftar or suhoor
GLP-1 receptor agonists
- no dose modifications
DPP-4 inhibitors
- no dose modifications
SGLT2 inhibitors
- no dose modifications
- dose should be taken with iftar
- extra clear fluids should be ingested during non-fasting periods
- should not be used in the elderly, people with renal impairment, hypotensive people or those taking diuretics
Long- or intermediate-acting basal insulin (5,6,7):
- OD – NPH/detemir/glargine/degludec. Take at iftar. Reduce dose by 15–30%
- BD – NPH/detemir/glargine. Swap usual dosing. Take usual morning dose at iftar. Reduce evening dose by 50% and take at suhoor
Rapid- or short-acting prandial/bolus insulin (5,6,7):
- take normal dose at iftar. Omit lunchtime dose. Reduce suhoor dose by 25–50%
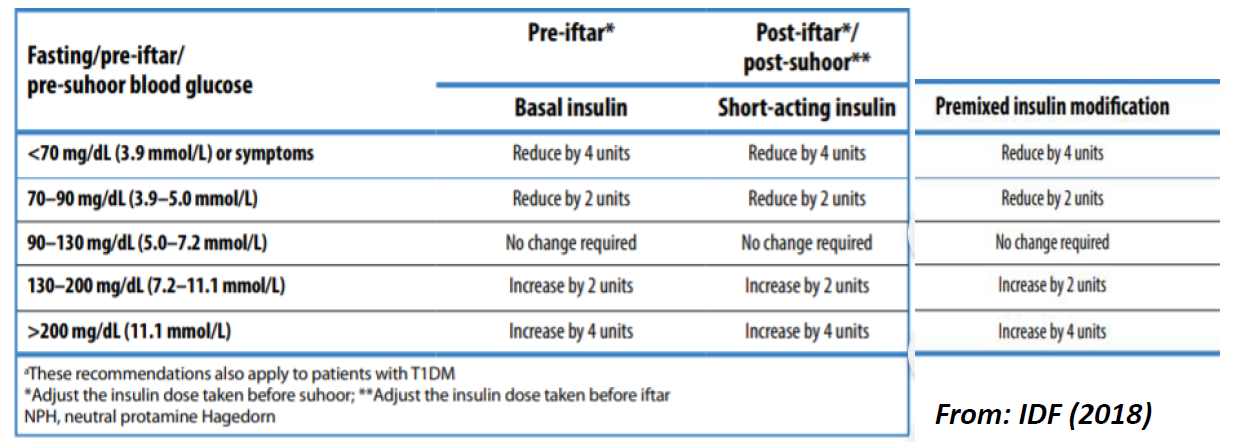
- dose titration should be performed every 3 days and adjustments made according to BG levels
Premixed insulin (5,6,7):
- OD – Take normal dose at iftar
- BD – If dose usually higher in morning, consider the higher dose at iftar and lower dose at suhoor. Take usual morning dose at iftar. Reduce evening dose 25–50% and take at suhoor
- TDS – Omit afternoon dose. Adjust iftar and suhoor doses according to blood glucose test
The patient should be also be advised (1):
- not to miss a meal at Souhar
- not to overeat at Iftar
- not to attempt self-reduction or omission of treatment
- to regularly monitor blood glucose during the fast
evidence suggests:
- there is an overall improvement in glycaemic control during the fast
- significant hypoglycaemia is unlikely on similar average doses of oral hypoglycaemic agents before and during Ramadan (1)
Reference:
- Pulse 2001; 61 (45): 96.
- Drug and Therapeutic Bulletin 2005; 43(10): 73-77.
- International Diabetes Federation (IDF), Diabetes and Ramadan (DAR) International Alliance (2016) Diabetes and Ramadan: Practical Guidelines. https://bit.ly/2kursXj
- Gilani A. How to manage diabetes in Ramadan. Diabetes & Primary Care 2019; 21: 41–2
- International Diabetes Federation:Diabetes and Ramadan Practical Guidelines (2018) https://www.idf.org/e-library/guidelines/87-diabetes-and-ramadanpractical- 25.html
- The South Asian Health Foundation (UK) Guidelines for Managing Diabetes During Ramadan: 2020 Update (2020) https://www.sahf.org.uk/resources
- NHS Sandwell and West Birmingham CCG (Accessed 23/9/2020). Summary fasting guidelines for Diabetes during Ramadan
- Mahmood A, Dar S, Dabhad A, Aksi B, Chowdhury T A. Advising patients with existing conditions about fasting during Ramadan BMJ 2022; 376 :e063613 doi:10.1136/bmj-2020-063613
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page