Investigation in testosterone deficiency
Blood tests - measurement of morning basal testosterone, LH, FSH, PRL - measurement of the basal levels of testosterone, LH and FSH will allow distinction between gonadal disease and hypothalamic-pituitary disease (1,2,3)
- primary hypogonadism - elevated gonadotrophin levels and low testosterone levels
- secondary hypogonadism - low to normal gonadotrophin levels and low testosterone levels
When considering a diagnosis of symptomatic TD, other blood investigations should include:
- haematocrit as part of FBC
- prostate specific antigen (PSA), with appropriate counselling
- Appropriate tests according to physical findings and to determine cardiovascular risk
Total testosterone (TT) should be measured before 11am with a reliable method, on at least two separate occasions, preferably 4 weeks apart. Fasting levels should be obtained where possible, as non-fasting levels may be up to 30% lower (3)If TT is low or borderline (<12 nmol/L):
- Measure sex hormone-binding globulin to calculate free testosterone (FT: an online FT calculator and downloadable app, sponsored by the Primary Care Testosterone Advisory Group, can be found at: http://www.pctag.uk/testosterone-calculator/)
- Measure serum luteinising hormone (LH) to differentiate primary from secondary TD.
- Measure follicle stimulating hormone (FSH) if fertility is an issue
Biopsy of the testes may be necessary for diagnosis but rarely reveals a treatable pathology.
Other investigations may be indicated and include:
- skull radiology including a pituitary CT scan
- semen analysis
- chromosomal analysis e.g. Klinefelter's disease
- bone age estimation
A suggested algorithm for assessment of possible testosterone deficiency in primary care:
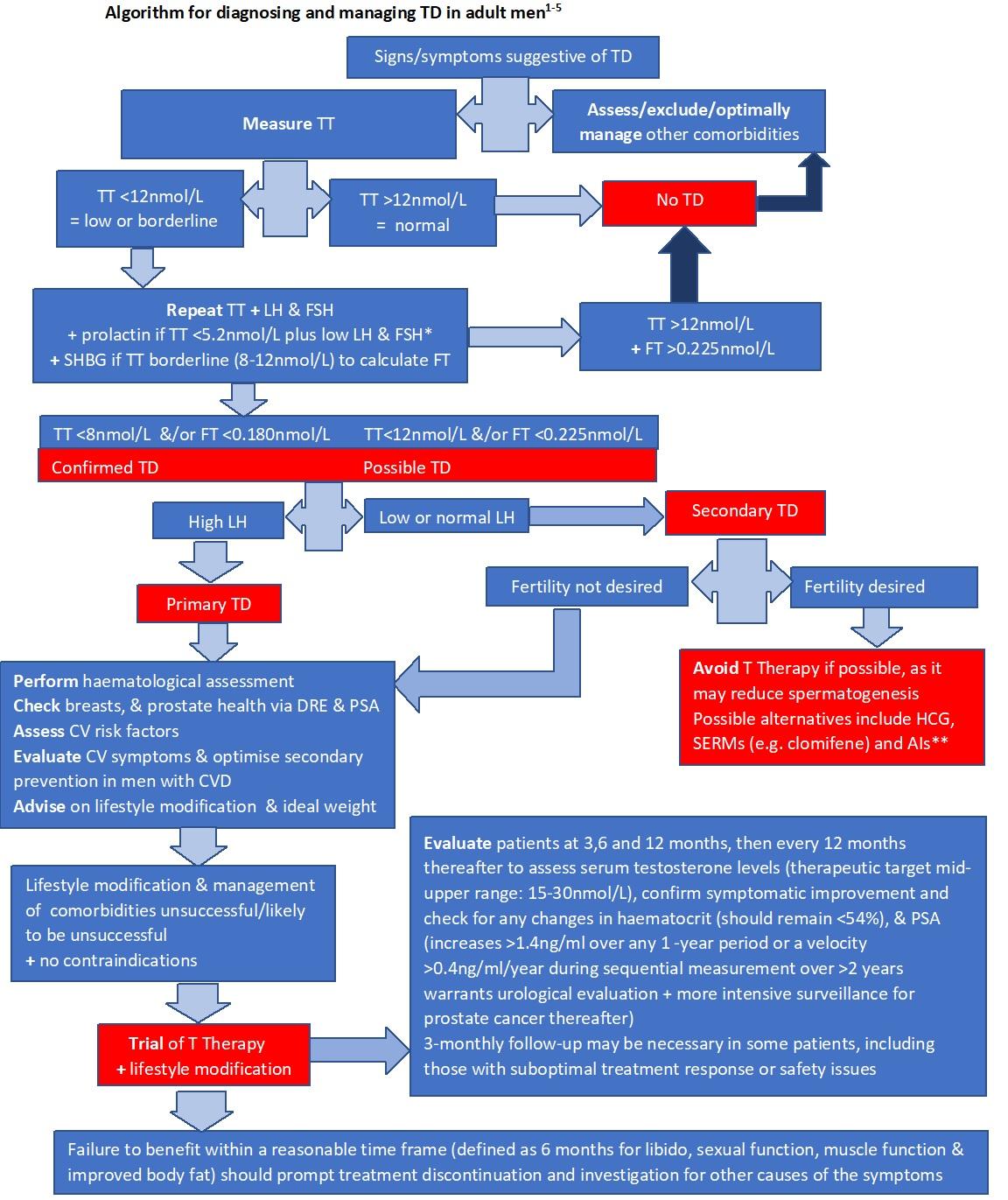
- Key points
- an acute illness may cause a fall in testosterone levels, therefore investigate suspected testosterone deficiency once any acute illness has fully resolved
- most discriminant symptoms associated with low testosterone (<12nmol/L) are: low libido, loss of early morning erections & erectile dysfunction - particularly in combination
- consider potentially reversible factors that may be causing a low testosterone, that can be addressed - concurrent illness, certain drugs (prescribed or otherwise e.g. ketoconazole, cimetidine, spironolactone, chemotherapy, opioids) and lifestyle factors (e.g. excessive alcohol; stress; significant weight gain/obesity, excessive exercise etc.).
- an acute illness may cause a fall in testosterone levels, therefore investigate suspected testosterone deficiency once any acute illness has fully resolved
References:
- Matsumoto AM. Diagnosis and evaluation of hypogonadism. Endocrinol Metab Clin North Am. 2022 Mar;51(1):47-62.
- Jayasena CN, Anderson RA, Llahana S, et al. Society for Endocrinology guidelines for testosterone replacement therapy in male hypogonadism. Clin Endocrinol (Oxf). 2022 Feb;96(2):200-19.
- Mulhall JP, Trost LW, Brannigan RE, et al. Evaluation and management of testosterone deficiency: AUA guideline. J Urol. 2018 Aug;200(2):423-32.
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page