Diabetic foot infection
Diabetic foot infection
Investigation
- if a diabetic foot infection is suspected and a wound is present, send a soft tissue or bone sample from the base of the debrided wound for microbiological
examination. If this cannot be obtained, take a deep swab because it may provide useful information on the choice of antibiotic treatment - consider an X-ray of the person's affected foot (or feet) to determine the extent of the diabetic foot problem
- think about osteomyelitis if the person with diabetes has a local infection, a deep foot wound or a chronic foot wound
- be aware that osteomyelitis may be present in a person with diabetes despite normal inflammatory markers, X-rays or probe-to-bone testing
- if osteomyelitis is suspected in a person with diabetes but is not confirmed by initial X-ray, consider an MRI to confirm the diagnosis
Treatment
- start antibiotic treatment for people with suspected diabetic foot infection as soon as possible. Take samples for microbiological testing before, or as close as possible to, the start of antibiotic treatment
- when choosing an antibiotic for people with a suspected diabetic foot infection, take account of:
- the severity of diabetic foot infection (mild, moderate or severe)
- the risk of developing complications
- previous microbiological results
- previous antibiotic use
- patient preferences
Severity of diabetic foot infection is defined by criteria below:
- Mild diabetic foot infection
- local infection involving only the skin and subcutaneous tissue; if erythema, must be 0.5 cm to less than 2 cm around the ulcer (exclude other causes of inflammatory response, such as trauma, gout, acute Charcot neuro-osteoarthropathy, fracture, thrombosis and venous stasis)
- Moderate diabetic foot infection
- local infection with erythema more than 2 cm around the ulcer or involving structures deeper than skin and subcutaneous tissues (such as abscess, osteomyelitis, septic arthritis or fasciitis), and no
systemic inflammatory response signs
- local infection with erythema more than 2 cm around the ulcer or involving structures deeper than skin and subcutaneous tissues (such as abscess, osteomyelitis, septic arthritis or fasciitis), and no
- Severe diabetic foot infection
- local infection with signs of systemic inflammatory response (such as temperature of more than 38°C or less than 36°C, increased heart rate or increased respiratory rate).
Choice of antibiotic:
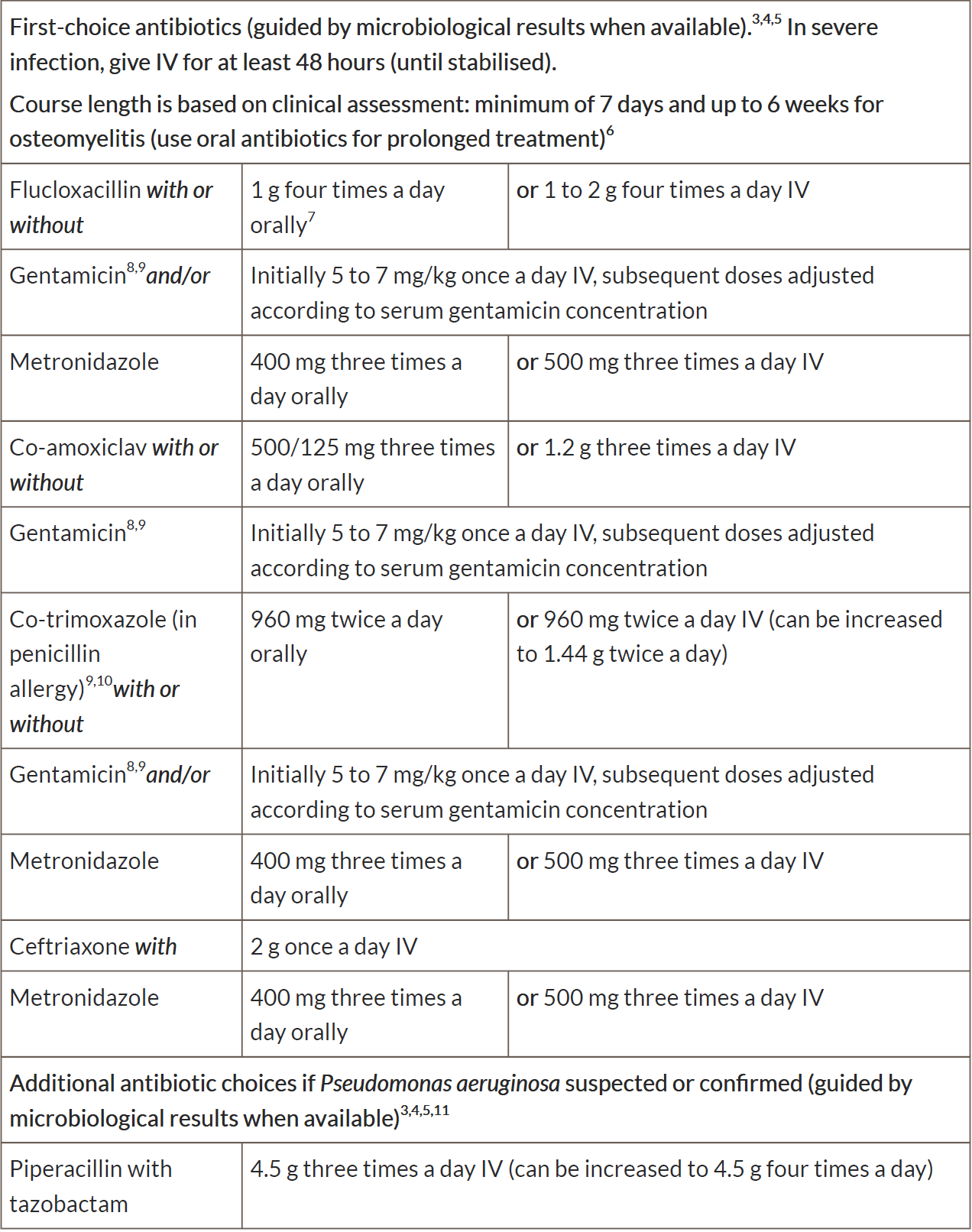
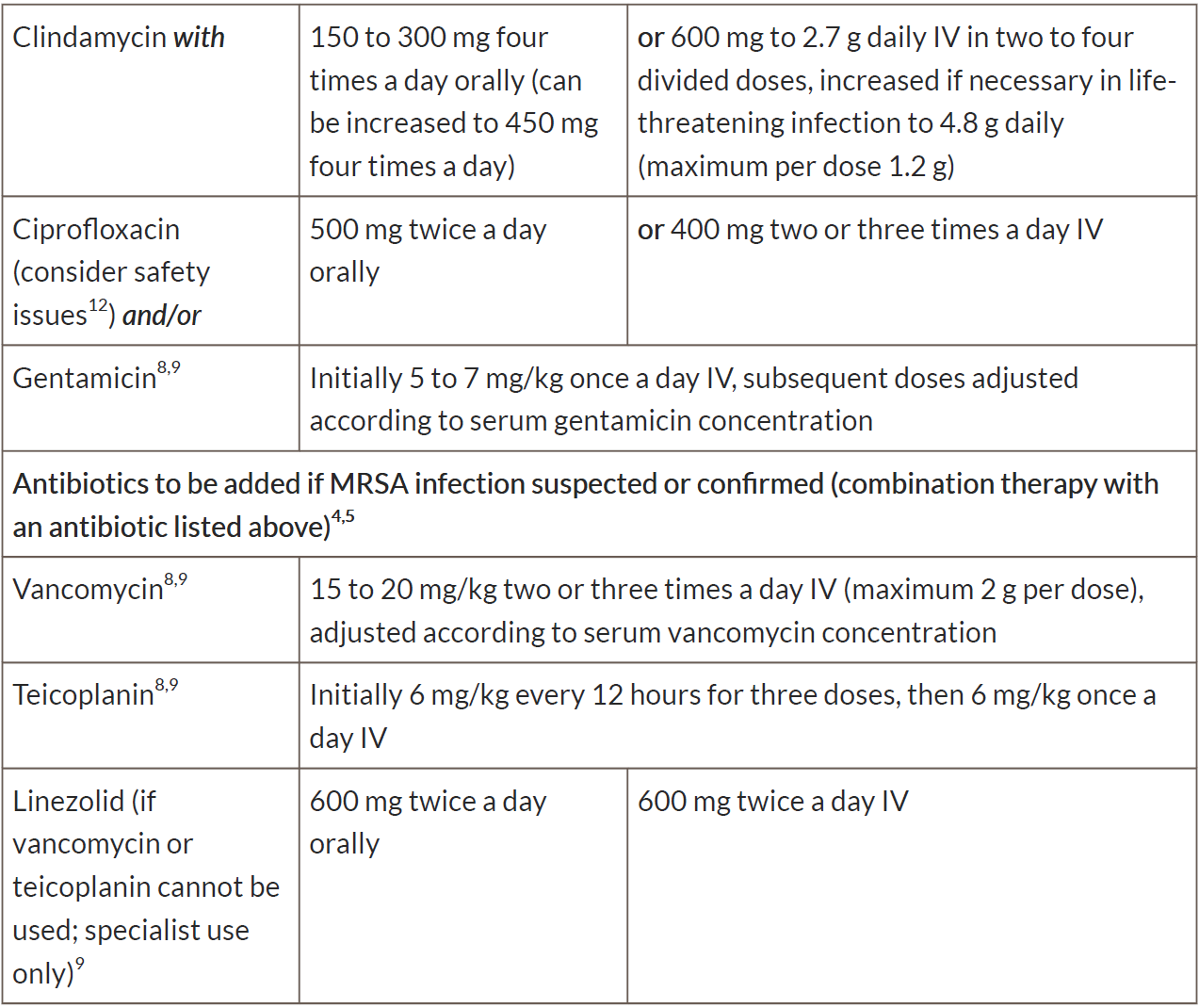
When prescribing antibiotics for a suspected diabetic foot infection in adults aged 18 years and over, follow table 1 for a mild infection or table 2 for a
moderate or severe infection.
Seek specialist advice when prescribing antibiotics for a suspected diabetic foot infection in children and young people under 18 years.
Give oral antibiotics first line if the person can take oral medicines, and the severity of their condition does not require intravenous antibiotics.
If intravenous antibiotics are given, review by 48 hours and consider switching to oral antibiotics if possible.
Base antibiotic course length on the severity of the infection and a clinical assessment of response to treatment. Review the need for continued antibiotics
regularly.
Table 1 Antibiotics for mild diabetic foot infection in adults aged 18 years and over
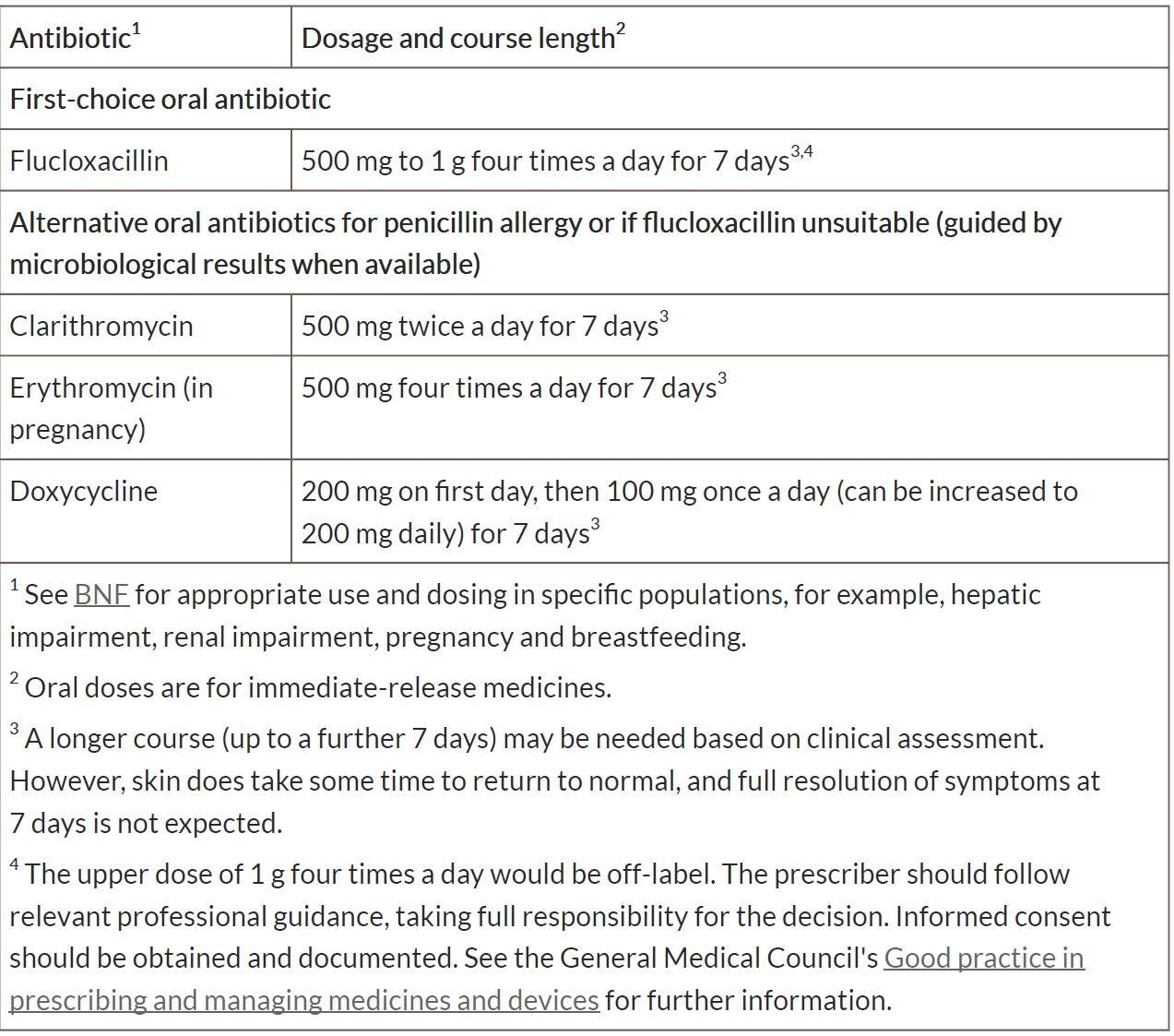
Table 2 Antibiotics for moderate or severe diabetic foot infection in adults aged 18 years and over
Advice
When prescribing antibiotics for a diabetic foot infection, give advice about:
- possible adverse effects of the antibiotic(s)
- seeking medical help if symptoms worsen rapidly or significantly at any time, or do not start to improve within 1 to 2 days
Reassessment
When microbiological results are available:
- review the choice of antibiotic and
- change the antibiotic according to results, using a narrow-spectrum antibiotic, if appropriate.
Reassess people with a suspected diabetic foot infection if symptoms worsen rapidly or significantly at any time, do not start to improve within 1 to 2 days, or
the person becomes systemically very unwell or has severe pain out of proportion to the infection. Take account of:
- other possible diagnoses, such as pressure sores, gout or non-infected ulcers
- any symptoms or signs suggesting a more serious illness or condition, such as limb ischaemia, osteomyelitis, necrotising fasciitis or sepsis
- previous antibiotic use
Key points (2):
- in diabetes, all foot wounds are likely to be colonised with bacteria. Diabetic foot infection has at least 2 of:
- local swelling or induration;
- erythema;
- local tenderness or pain;
- local warmth;
- purulent discharge
- severity is classified as:
- Mild:
- local infection with 0.5 to less than 2cm erythema
- Moderate:
- local infection with more than 2cm erythema or involving deeper structures (such as abscess, osteomyelitis, septic arthritis or fasciitis)
- Severe:
- local infection with signs of a systemic inflammatory response
- Mild:
- start antibiotic treatment as soon as possible. Take samples for microbiological testing before, or as close as possible to, the start of treatment
- when choosing an antibiotic, take account of severity, risk of complications, previous microbiological results and antibiotic use, and patient preference
- *a longer course (up to a further 7 days) may be needed based on clinical assessment. However, skin does take time to return to normal, and full resolution at 7 days is not expected
- do not offer antibiotics to prevent diabetic foot infection.
Reference:
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page