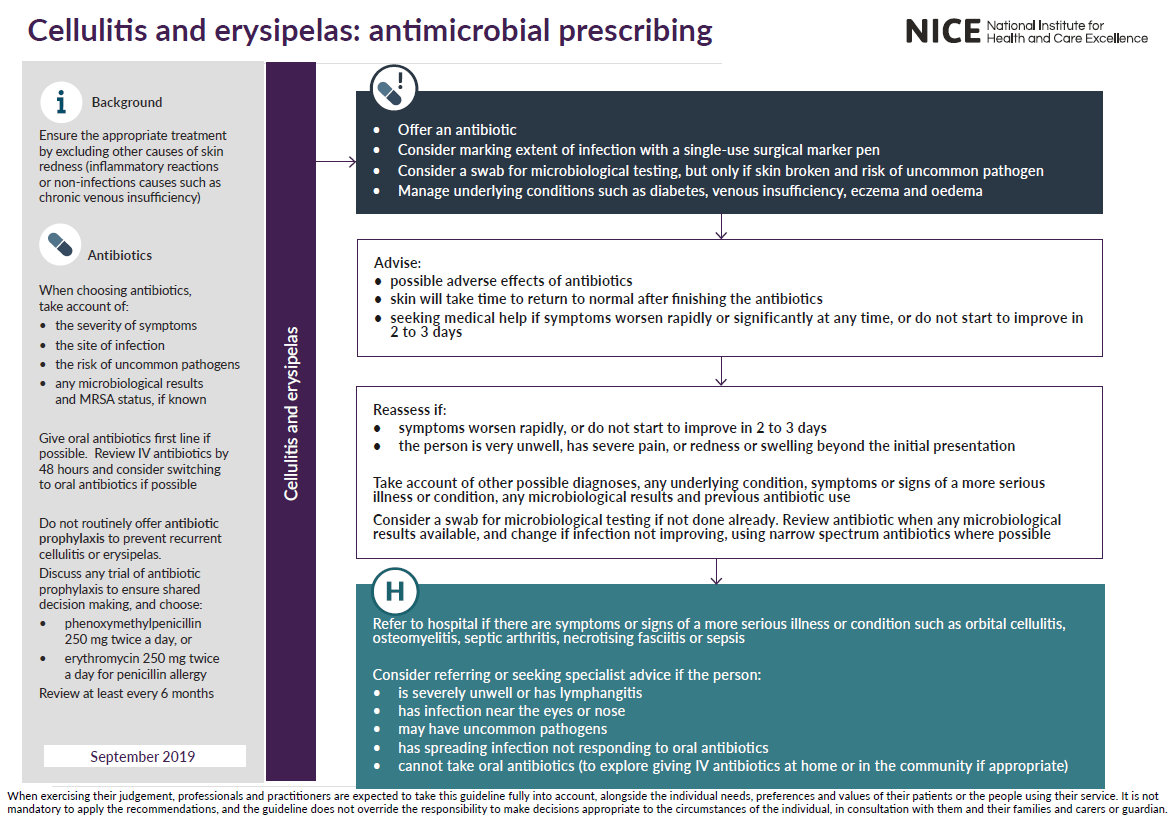
Management of cellulitis or erysipelas - including principles of antibiotic prescribing
Management of cellulitis or erysipelas
Consider taking a swab for microbiological testing from people with cellulitis or erysipelas to guide treatment, but only if the skin is broken and:
- there is a penetrating injury or
- there has been exposure to water-borne organisms or
- the infection was acquired outside the UK
Before treating cellulitis or erysipelas, consider drawing around the extent of the infection with a single-use surgical marker pen to monitor progress. Be aware that redness may be less visible on darker skin tones
Manage any underlying condition that may predispose to cellulitis or erysipelas, for example:
- diabetes
- venous insufficiency
- eczema
- oedema, which may be an adverse effect of medicines such as calcium channel blockers.
Reassessment
- reassess people with cellulitis or erysipelas if symptoms worsen rapidly or significantly at any time, do not start to improve within 2 to 3 days, or the person:
- becomes systemically very unwell or
- has severe pain out of proportion to the infection or
- has redness or swelling spreading beyond the initial presentation (taking into account that some initial spreading may occur, and that redness may be less visible on darker skin tones)
When reassessing people with cellulitis or erysipelas, take account of:
- other possible diagnoses, such as an inflammatory reaction to an immunisation or an insect bite, gout, superficial thrombophlebitis, eczema, allergic dermatitis or deep vein thrombosis
- any underlying condition that may predispose to cellulitis or erysipelas, such as oedema, diabetes, venous insufficiency or eczema
- any symptoms or signs suggesting a more serious illness or condition, such as lymphangitis, orbital cellulitis, osteomyelitis, septic arthritis, necrotising fasciitis or sepsis
- any results from microbiological testing
- any previous antibiotic use, which may have led to resistant bacteria.
Consider taking a swab for microbiological testing from people with cellulitis or erysipelas if the skin is broken and this has not been done already.
If a swab has been sent for microbiological testing:
- review the choice of antibiotic(s) when results are available and
- change the antibiotic(s) according to results if symptoms or signs of the infection are not improving, using a narrow-spectrum antibiotic if possible.
Referral and seeking specialist advice
Refer people to hospital if they have any symptoms or signs suggesting a more serious illness or condition, such as orbital cellulitis, osteomyelitis, septic arthritis, necrotising fasciitis or sepsis. Consider referring people with cellulitis or erysipelas to hospital, or seek specialist advice, if they:
- are severely unwell or have infection near the eyes or nose (including periorbital cellulitis) or
- could have uncommon pathogens, for example, after a penetrating injury, exposure to water-borne organisms, or
- an infection acquired outside the UK or
- have spreading infection that is not responding to oral antibiotics or
- lymphangitis or
- cannot take oral antibiotics (exploring locally available options for giving intravenous antibiotics at home or in the community, rather than in hospital, where appropriate).
Summary of NICE assessment and review advice (1):
Antibiotics for adults aged 18 years and over:
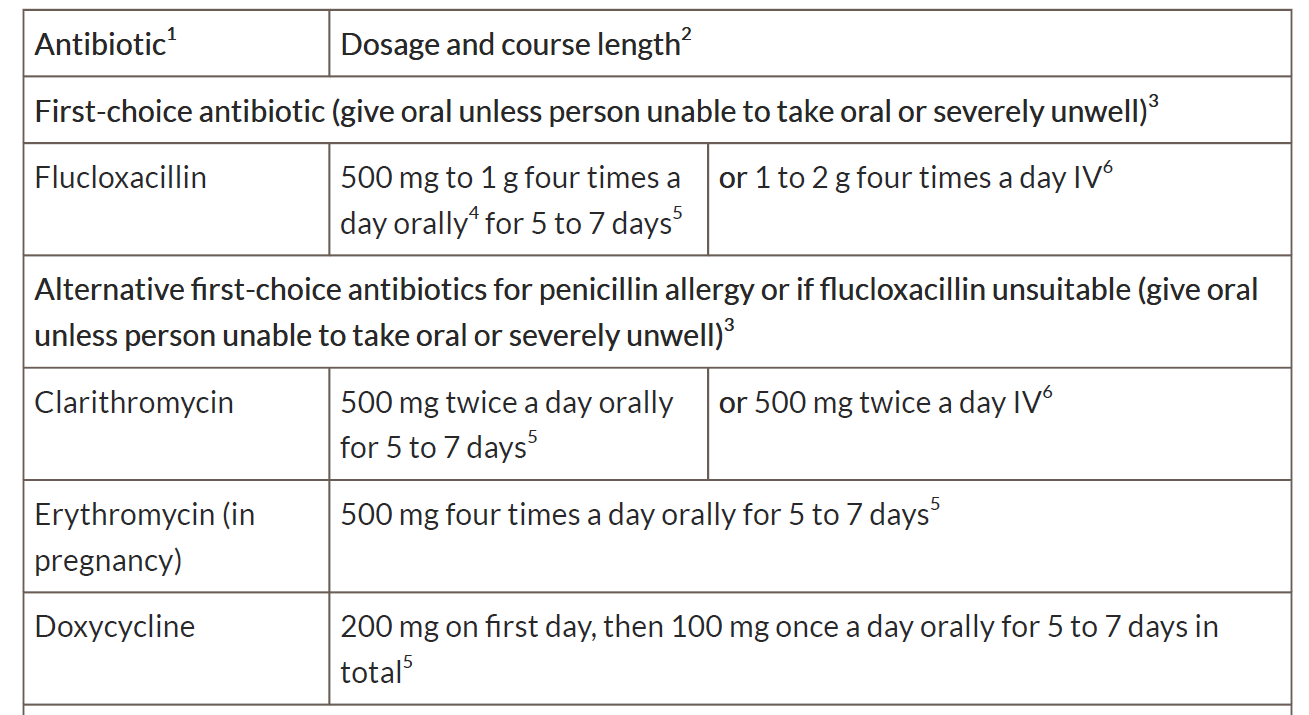
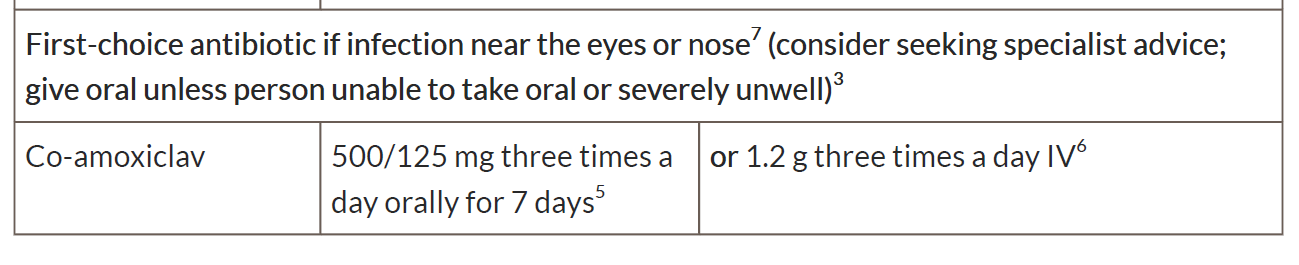
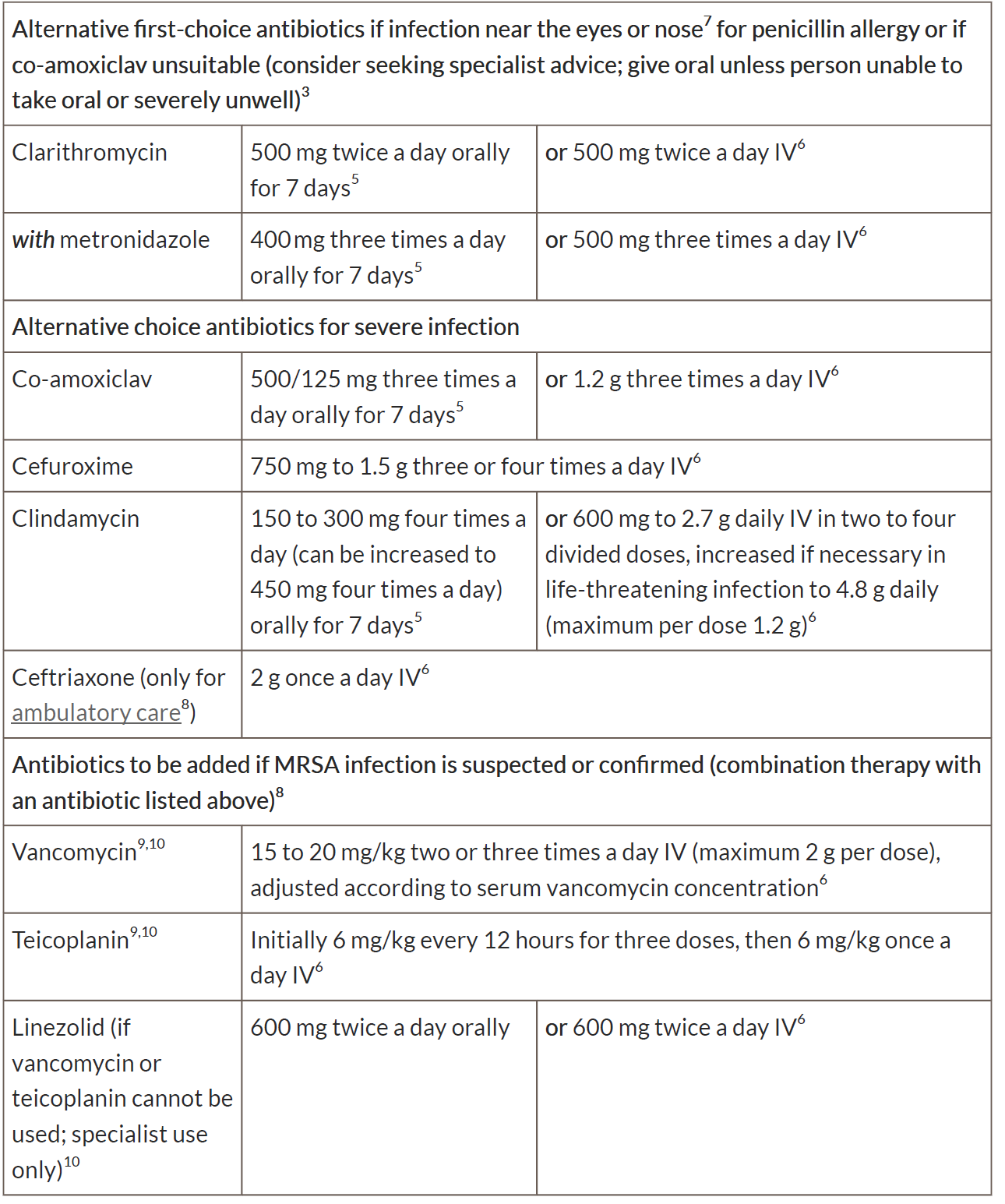
1See BNF for appropriate use and dosing in specific populations, for example, hepatic impairment, renal impairment, pregnancy and breastfeeding, and administering intravenous (or, where appropriate, intramuscular) antibiotics.
2 Oral doses are for immediate-release medicines.
3 Give oral antibiotics first line if the person can take oral medicines, and the severity of their symptoms does not require intravenous antibiotics.
4 The upper dose of 1 g four times a day would be off-label. The prescriber should follow relevant professional guidance, taking full responsibility for the decision. Informed consent should be obtained and documented. See the General Medical Council's Good practice in prescribing and managing medicines and devices for further information.
5 A longer course (up to 14 days in total) may be needed based on clinical assessment. However, skin does take some time to return to normal, and full resolution of symptoms at 5 to 7 days is not expected.
6 If intravenous antibiotics are given, review by 48 hours and consider switching to oral antibiotics if possible for the appropriate course length.
7 Infection around the eyes or the nose (the triangle from the bridge of the nose to the corners of the mouth, or immediately around the eyes including periorbital cellulitis) is of more concern because of risk of a serious intracranial complication.
8 Other antibiotics may be appropriate based on microbiological results and specialist advice.
9 See BNF for information on therapeutic drug monitoring.
10 See BNF for information on monitoring of patient parameters.
Reference:
- Cellulitis and erysipelas: antimicrobial prescribing. NICE guideline NG141. Published: 27 September 2019
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page