Prognosis of CML
Tyrosine kinase inhibitors have significantly improved the prognoses for CML patients. Since their introduction as first-line treatment options for CML, five-year survival has risen from 33% to over 90%. (1)
Ten-year survival has risen from 11% to 84%, and complete cytogenetic response occurs in 70% to 90% of patients.
People diagnosed with chronic phase CML are expected to reach normal or near-normal life expectancy. (2)
Surveillance, Epidemiology, and End Results (SEER) Program data (2000-2020) report the following relative survival rates (all stages) by time since diagnosis: (3)
77.9% (2-year survival)
66.8% (5-year survival)
58% (10-year survival)
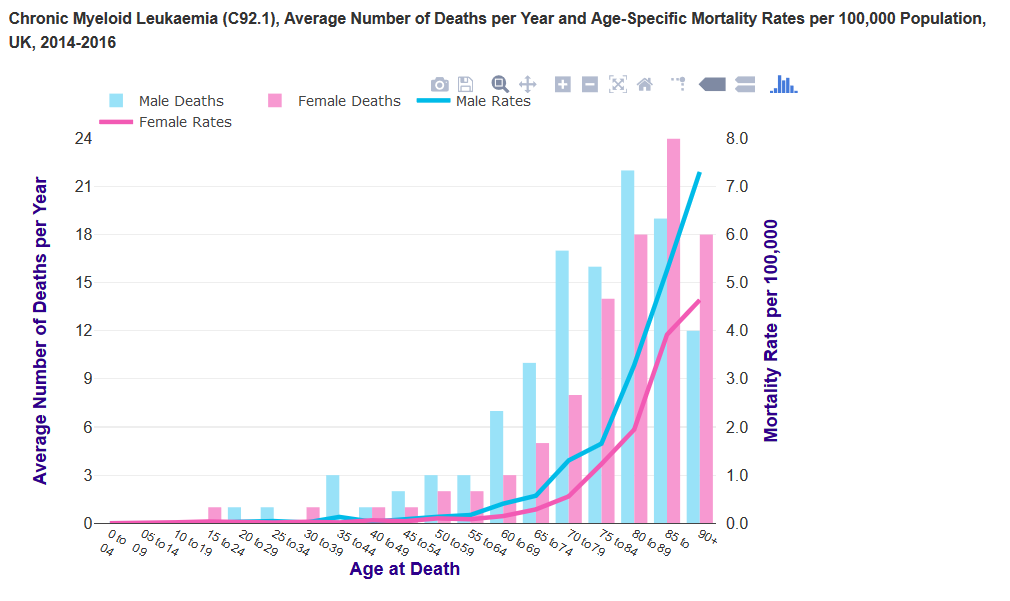
Prognosis is poorer for older patients with CML. 5-year relative survival rates (all stages; 2000-2020) by time since diagnosis:
<50 years: 87.5%
50-64 years: 78.2%
≥65 years: 44.7%
The prognosis for patients with blast crisis remains poor, particularly for patients with progression from chronic phase chronic myeloid leukaemia (CML) or with myeloid phenotype blast crisis. (4)
It is important to identify the prognostic factors at diagnosis. The following can be used to provide useful prognostic information in a patient with CML:
- accurate identification of the disease stage (or phase) is considered to be the essential factor
- clinical and laboratory features - used to calculate prognostic scores (Sokal score or Hasford score)
- these scores identifies patients with low, intermediate, and high risk of short term survival
- cytogenetic changes e.g. - deletions of the derivative chromosome 9
- Imatinib can be used to partly overcome the negative prognostic effects of this
- but the size and location of the deletion appears to be important
- degree and timing of haematological, cytogenetic, and molecular responses
Approximately 60% of young adults with successful allogeneic bone marrow transplantation are cured.
References:
- Fava C, Rege-Cambrin G, Saglio G. The choice of first-line chronic myelogenous leukemia treatment. Ann Hematol. 2015 Apr;94 Suppl 2:S123-31.
- Eden R. Chronic Myelogenous Leukemia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan.2023 Jan 16.
- National Cancer Institute. Surveillance, Epidemiology, and End Results Program. SEER explorer [internet publication].
- Jain P, Kantarjian HM, Ghorab A, et al. Prognostic factors and survival outcomes in patients with chronic myeloid leukemia in blast phase in the tyrosine kinase inhibitor era: cohort study of 477 patients. Cancer. 2017 Nov 15;123(22):4391-402.
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page