Management of STEMI
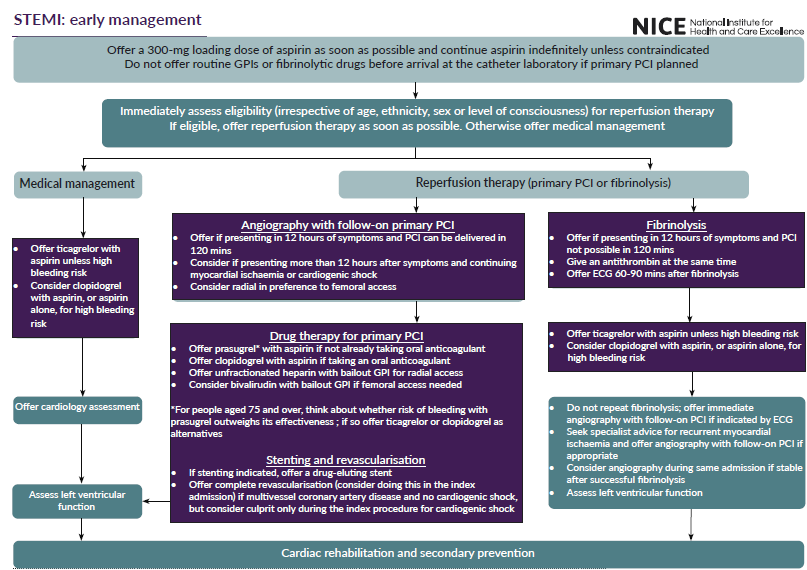
STEMI - early management
Assessment
- immediately assess eligibility (irrespective of age, ethnicity or sex) for coronary reperfusion therapy (either primary percutaneous coronary intervention [PCI] or fibrinolysis) in people with acute ST-segment elevation myocardial infarction (STEMI)
- do not use level of consciousness after cardiac arrest caused by suspected acute STEMI to determine whether a person is eligible for coronary angiography (with follow-on primary PCI if indicated)
- deliver coronary reperfusion therapy (either primary PCI or fibrinolysis) as quickly as possible for eligible people with acute STEMI
Initial drug therapy
- offer people with acute STEMI a single loading dose of 300-mg aspirin as soon as possible unless there is clear evidence that they are allergic to it.
- do not offer routine glycoprotein IIb/IIIa inhibitors or fibrinolytic drugs before arrival at the catheter laboratory to people with acute STEMI for whom primary PCI is planned
Coronary angiography with follow-on primary PCI
- offer coronary angiography, with follow-on primary PCI if indicated, as the preferred coronary reperfusion strategy for people with acute STEMI, if:
- presentation is within 12 hours of onset of symptoms and
- primary PCI can be delivered within 120 minutes of the time when fibrinolysis could have been given
- offer coronary angiography, with follow-on primary PCI if indicated, to people with acute STEMI and cardiogenic shock who present within 12 hours of the onset of symptoms of STEMI
- consider coronary angiography, with follow-on primary PCI if indicated, for people with acute STEMI presenting more than 12 hours after the onset of symptoms if there is evidence of continuing myocardial ischaemia
- consider coronary angiography, with a view to coronary revascularisation if indicated, for people with acute STEMI who present more than 12 hours after the onset of symptoms and who have cardiogenic shock or go on to develop it
- consider radial (in preference to femoral) arterial access for people undergoing coronary angiography (with follow-on primary PCI if indicated)
Dual antiplatelet therapy for people with acute STEMI having primary PCI
For people with acute STEMI who are having primary PCI, offer:
- Prasugrel, as part of dual antiplatelet therapy with aspirin, if they are not already taking an oral anticoagulant (use the maintenance dose in the prasugrel summary of product characteristics; for people aged 75 and over, think about whether the person's risk of bleeding with prasugrel outweighs its effectiveness, in which case offer ticagrelor or clopidogrel as alternatives)
- Clopidogrel, as part of dual antiplatelet therapy with aspirin, if they are already taking an oral anticoagulant
Antithrombin therapy during primary PCI
- offer unfractionated heparin with bailout glycoprotein IIb/IIIa inhibitor in combination with dual antiplatelet therapy to people with acute STEMI undergoing primary PCI with radial access
- consider bivalirudin with bailout glycoprotein IIb/IIIa inhibitor in combination with dual antiplatelet therapy for people with acute STEMI undergoing primary PCI when femoral access is needed.
In November 2020, use of bivalirudin with prasugrel and aspirin was off label. See NICE's information on prescribing medicines
Thrombus extraction during primary PCI
- consider thrombus aspiration during primary PCI for people with acute STEMI
- do not routinely use mechanical thrombus extraction during primary PCI for people with acute STEMI
Complete or culprit vessel only revascularisation with PCI in people with acute STEMI treated by primary PCI
- offer complete revascularisation with PCI for people with acute STEMI and multivessel coronary artery disease without cardiogenic shock. Consider doing this during the index hospital admission
- consider culprit vessel only revascularisation with PCI rather than complete revascularisation during the index procedure for people with acute STEMI and multivessel coronary artery disease with cardiogenic shock
Drug-eluting stents in primary PCI
- if stenting is indicated, offer a drug-eluting stent to people with acute STEMI undergoing revascularisation by primary PCI
Fibrinolysis
- offer fibrinolysis to people with acute STEMI presenting within 12 hours of onset of symptoms if primary PCI cannot be delivered within 120 minutes of the time when fibrinolysis could have been given
- when treating people with fibrinolysis, give an antithrombin at the same time
- offer an electrocardiogram (ECG) to people with acute STEMI treated with fibrinolysis, 60 to 90 minutes after administration. For those who have residual ST-segment elevation suggesting failed coronary reperfusion:
- offer immediate coronary angiography, with follow-on PCI if indicated
- do not repeat fibrinolytic therapy
- if a person with acute STEMI has recurrent myocardial ischaemia after fibrinolysis, seek immediate specialist cardiological advice and, if appropriate, offer coronary angiography, with follow-on PCI if indicated
- consider coronary angiography during the same hospital admission for people with acute STEMI who are clinically stable after successful fibrinolysis
Management for people with STEMI not treated with PCI
- offer ticagrelor, as part of dual antiplatelet therapy with aspirin, to people with acute STEMI not treated with PCI, unless they have a high bleeding risk
- consider clopidogrel, as part of dual antiplatelet therapy with aspirin, or aspirin alone, for people with acute STEMI not treated with PCI, if they have a high bleeding risk
Offer medical management to people with acute STEMI who are ineligible for any reperfusion therapy
Tests before discharge
- assess left ventricular function in all people who have had a STEMI
Reference:
- NICE. Acute coronary syndromes. NICE guideline NG185. Published: 18 November 2020.
Related pages
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page