Investigation of possible angina
Investigation of possible angina (1):
- if the estimated likelihood of CAD is less than 10% (see tables below), first consider causes of chest pain other than angina caused by CAD
- consider investigating other causes of angina, such as hypertrophic cardiomyopathy, in people with typical angina-like chest pain and a low likelihood of CAD (estimated at less than 10%)
- arrange blood tests to identify conditions which exacerbate angina, such as anaemia, for all people being investigated for stable angina
- only consider chest X-ray if other diagnoses, such as a lung tumour, are suspected
- if a diagnosis of stable angina has been excluded, but people have risk factors for cardiovascular disease, then address these e.g. hypertension, raised lipids
- for people in whom stable angina cannot be diagnosed or excluded on the basis of the clinical assessment alone, take a resting 12-lead ECG as soon as possible after presentation
- do not rule out a diagnosis of stable angina on the basis of a normal resting 12-lead ECG
- a number of changes on a resting 12-lead ECG are consistent with CAD and may indicate ischaemia or previous infarction. These include:
- pathological Q waves in particular
- LBBB
- ST-segment and T wave abnormalities (for example, flattening or inversion). Note that the results may not be conclusive. Consider any resting 12-lead ECG changes together with people's clinical history and risk factors
- for people with confirmed CAD (for example, previous MI, revascularisation, previous angiography) in whom stable angina cannot be diagnosed or excluded based on clinical assessment alone, consider functional testing - an exercise ECG may be used as an alternative to functional testing (ie exercise ECG as a diagnostic tool only if person has a diagnosis of CAD already)
- in people without confirmed CAD, in whom stable angina cannot be diagnosed or excluded based on clinical assessment alone, estimate the likelihood of CAD (see tables). Take the clinical assessment and the resting 12-lead ECG into account when making the estimate. Arrange further diagnostic testing as follows:
- if the estimated likelihood of CAD is 61-90%, offer invasive coronary angiography as the first-line diagnostic investigation if appropriate
- if the estimated likelihood of CAD is 30-60%, offer functional imaging as the first-line diagnostic investigation
- if the estimated likelihood of CAD is 10-29%, offer CT calcium scoring as the first-line diagnostic investigation
- consider aspirin only if the person's chest pain is likely to be stable angina, until a diagnosis is made. Do not offer additional aspirin if there is clear evidence that people are already taking aspirin regularly or are allergic to it
- follow local protocols for stable angina while waiting for the results of investigations if symptoms are typical of stable angina
Table 1: Non-anginal chest pain - % likelihood of CAD
Men | Men | Women | Women | |
Age (years) | Lo | Hi | Lo | Hi |
35 | 3% | 35% | 1% | 19% |
45 | 9% | 47% | 2% | 22% |
55 | 23% | 59% | 4% | 45% |
65 | 49% | 69% | 9% | 49% |
Table 1 represents people with symptoms of non-anginal chest pain, who would not be investigated for stable angina routinely
Table 2: Atypical anginal pain - % likelihood of CAD
Men | Men | Women | Women | |
Age (years) | Lo | Hi | Lo | Hi |
35 | 8% | 59% | 2% | 39% |
45 | 21% | 70% | 5% | 43% |
55 | 45% | 79% | 10% | 47% |
65 | 71% | 86% | 20% | 51% |
Table 3: Typical angina - % likelihood of CAD
Men | Men | Women | Women | |
Age (years) | Lo | Hi | Lo | Hi |
35 | 30% | 88% | 10% | 78% |
45 | 51% | 92% | 20% | 79% |
55 | 80% | 95% | 38% | 82% |
65 | 93% | 97% | 56% | 84% |
- for men older than 70 with atypical or typical symptoms, assume an estimate > 90%.
- For women older than 70, assume an estimate of 61-90% EXCEPT women at high risk AND with typical symptoms where a risk of > 90% should be assumed
- Values are per cent of people at each mid-decade age with significant coronary artery disease (CAD)
- Hi = High risk = diabetes, smoking and hyperlipidaemia (total cholesterol > 6.47 mmol/litre)
- Lo = Low risk = none of these three
- Note:
- These results are likely to overestimate CAD in primary care populations. If there are resting ECG ST-T changes or Q waves, the likelihood of CAD is higher in each cell of the table.
NICE guidance (1):
Diagnostic testing for people in whom stable angina cannot be diagnosed or excluded by clinical assessment alone
Most people diagnosed with non-anginal chest pain after clinical assessment need no further diagnostic testing. However in a very small number of people, there are remaining concerns that the pain could be ischaemic, in which case the risk of undiagnosed angina outweighs the risk of any potential radiation exposure:
- include the typicality of anginal pain features and the estimate of CAD likelihood in all requests for diagnostic investigations and in the person's notes
- use clinical judgement and take into account people's preferences and comorbidities when considering diagnostic testing
- take into account people's risk from radiation exposure when considering which diagnostic test to use
- for people with chest pain in whom stable angina cannot be diagnosed or excluded by clinical assessment alone and who have an estimated likelihood of CAD of 61-90%, offer invasive coronary angiography after clinical assessment and a resting 12-lead ECG if:
- coronary revascularisation is being considered and
- invasive coronary angiography is clinically appropriate and acceptable to the person
- for people with chest pain in whom stable angina cannot be diagnosed or excluded by clinical assessment alone and who have an estimated likelihood of CAD of 61-90%, offer non-invasive functional imaging after clinical assessment and a resting 12-lead ECG if:
- coronary revascularisation is not being considered or
- invasive coronary angiography is not clinically appropriate or acceptable to the person
- for people with chest pain in whom stable angina cannot be diagnosed or excluded by clinical assessment alone and who have an estimated likelihood of CAD of 30-60% , offer non-invasive functional imaging for myocardial ischaemia
- for people with chest pain in whom stable angina cannot be diagnosed or excluded by clinical assessment alone and who have an estimated likelihood of CAD of 10-29% offer CT calcium scoring. If the calcium score is:
- zero, consider other causes of chest pain
- 1-400, offer 64-slice (or above) CT coronary angiography
- greater than 400, offer invasive coronary angiography. If this is not clinically appropriate or acceptable to the person and revascularisation is not being considered, offer non-invasive functional imaging
- for people with confirmed CAD (for example, previous MI, revascularisation, previous angiography), offer non-invasive functional testing when there is uncertainty about whether chest pain is caused by myocardial ischaemia. An exercise ECG may be used instead of functional imaging
When Additional diagnostic investigations are indicated
- non-invasive functional imaging should be offered for myocardial ischaemia if invasive coronary angiography or 64-slice (or above) CT coronary angiography has shown CAD of uncertain functional significance
- invasive coronary angiography should be offered as a second-line investigation when the results of non-invasive functional imaging are inconclusive
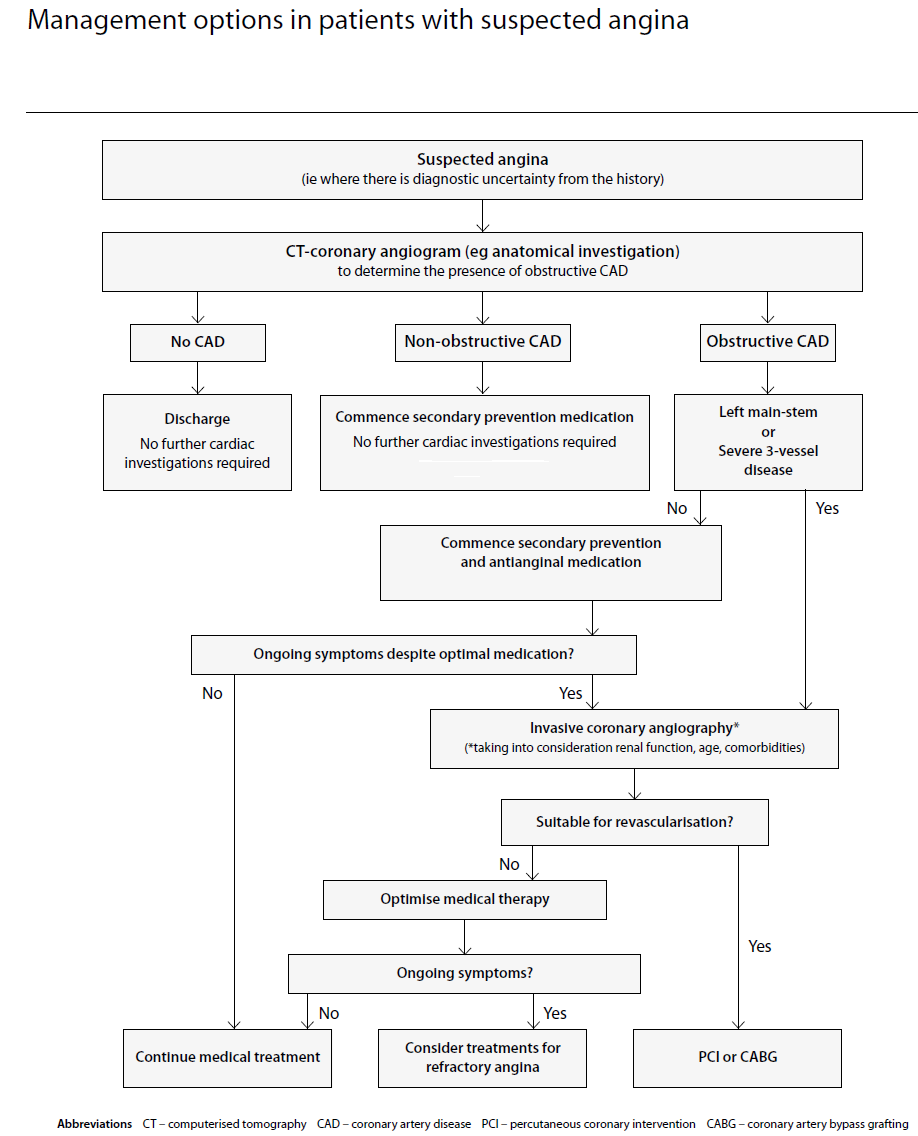
SIGN have outlined the management options in suspected angina (1):
- computerised tomography-coronary angiography should be considered for the initial investigation of patients with chest pain in whom the diagnosis of stable angina is suspected but not clear from history alone
- in patients with suspected stable angina, the exercise tolerance test should not be used routinely as a first-line diagnostic tool
- coronary angiography should be considered after non-invasive testing where patients are identified to be at high risk or where a diagnosis remains unclear
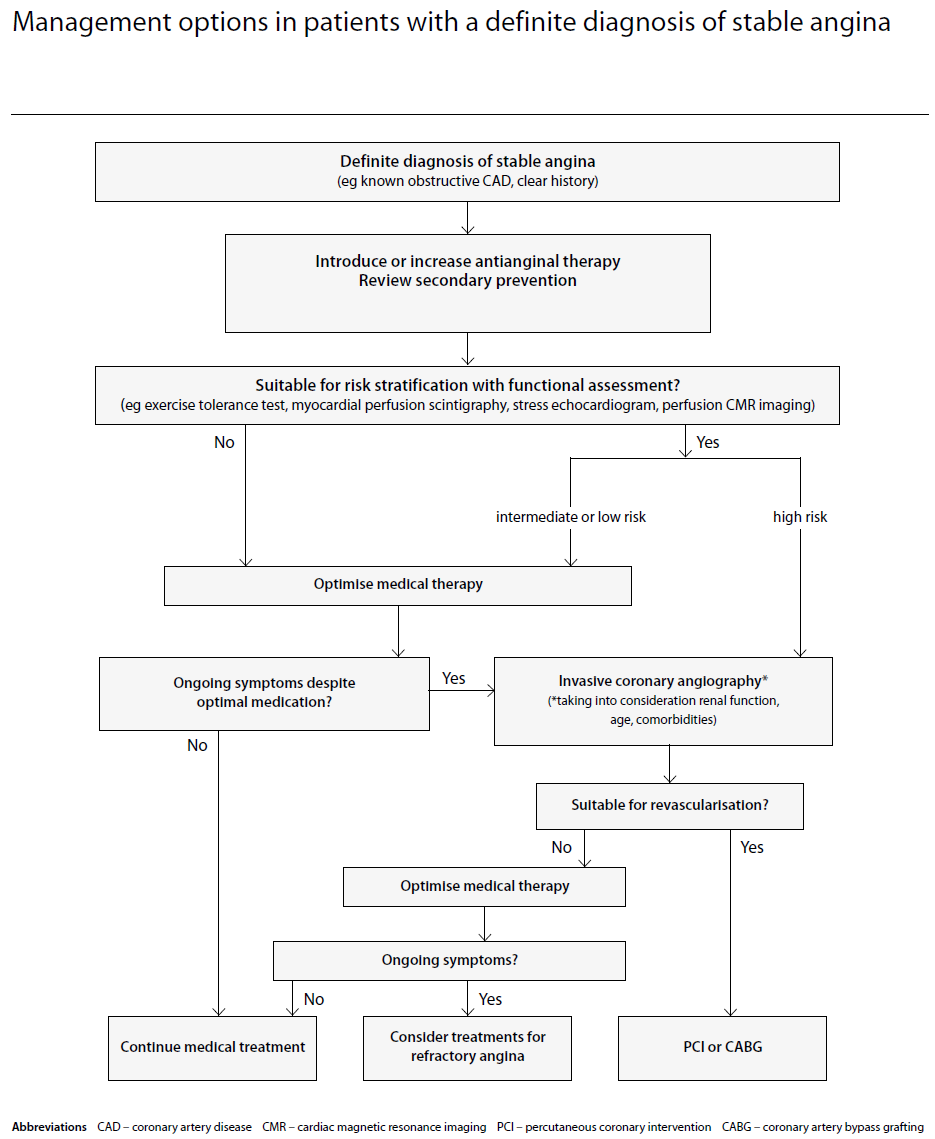
If assessing known stable angina (2):
Reference:
- NICE CKS, November 2020. Angina
- SIGN (April 2018). Management of Stable Angina.
Related pages
- Making a diagnosis of stable angina (coronary artery disease (CAD)) - what investigations are required
- Non-invasive functional testing for possible myocardial ischaemia
- Blood tests in angina
- ECG changes in angina
- Myocardial perfusion scintigraphy
- CT calcium scoring
- Coronary angiography
- Stress echocardiography
- Referral criteria from primary care - stable angina
Create an account to add page annotations
Add information to this page that would be handy to have on hand during a consultation, such as a web address or phone number. This information will always be displayed when you visit this page