Asthma is 'work-related' when there is an association between symptoms and work. The different types of work-related asthma should be distinguished, since the implications to the worker and the occupational health management of the disease differ
Work-related asthma includes two distinct categories:
- work aggravated asthma, i.e. pre-existing or coincidental new onset adult asthma which is made worse by non-specific factors in the workplace, and
- occupational asthma i.e. adult asthma caused by workplace exposure and not by factors outside of the workplace. Occupational asthma can occur in workers with or without prior asthma
- occupational asthmacan be further subdivided into:
- sensitiser-induced occupational asthmacharacterised by a latency period between first exposure to a respiratory sensitiser at work and the development of immunologically-mediated symptoms
- irritant-induced occupational asthma that occurs typically within a few hours of a high concentration exposure to an irritant gas, fume or vapour at work (1)
- workplace agents that induce asthma through an allergic mechanism can be broadly divided into those of high and low molecular weight
- the former are usually proteins and appear to act through a type I, IgE associated hypersensitivity.
- some low molecular weight chemicals are associated with the development of specific IgE antibodies, this is not the case for the majority
- almost 90% of cases of occupational asthma are of the allergic type
Occupational factors account for about 1 in 10 cases of asthma in adults of working age (4)
- Health and Safety Executive (HSE) estimate that 1,500 to 3,000 people develop occupational asthma each year. This rises to 7,000 cases a year if work-aggravated asthma is included
- it is thought that thereported incidence of occupational asthma is underestimated by about 50% (3)
- it is the commonest industrial lung disease in the developed world with over 400 reported causes (2)
- most frequently reported agents include isocyanates, flour and grain dust, colophony and fluxes, latex, animals, aldehydes and wood dust
- workers most commonly reported to surveillance schemes of occupational asthma include paint sprayers, bakers and pastry makers, nurses, chemical workers, animal handlers, welders, food processing and timber workers
- high risk work includes (2)
- baking
- pastry making
- spray painting
- laboratory animal work
- healthcare
- dentalcare
- food processing
- welding
- soldering
- metalwork
- woodwork
- chemical processing
- textile, plastics and rubber manufacture
- farming and other jobs with exposure to dusts and fumes
- smoking has been identified to increase the risk of occupational asthma in workers exposed to: isocyanates, platinum salts, salmon and snow crab
Occupational rhinitis and occupational asthma frequently occur as co-morbid conditions (1)
- epidemiological evidence from the general population of a strong association between the development of asthma and a previous history of either allergic or perennial rhinitis. Occupational rhinitis is purported to be a risk factor for the development of occupational asthma, especially for high-molecular-weight sensitisers
- rhino-conjunctivitis is more likely to appear before the onset of IgE associated occupational asthma
- risk of developing occupational asthma is highest in the year after the onset of occupational rhinitis
Diagnosis of occupational asthma
- occupational asthma should be suspected in all workers with symptoms of airflow limitations (2)
- the following screening questions could be useful in patients with airflow obstructions:
- are you better on days away from work?
- are you better on holiday?
- patients with a positive answer should be considered as having occupational asthma and should be investigated (2)
- made most easily before exposures or treatments are modified
- serial measurement of peak expiratory flow is the most available initial investigation
- minimum standards for diagnostic sensitivity >70% and specificity >85% are:
- at least three days in each consecutive work period
- at least three series of consecutive days at work with three periods away from work (usually about three weeks)
- at least four evenly spaced readings per day (2)
- when done and interpreted to validated standards there are very few false positive results, but about 20% are false negatives
- skin prick tests or blood tests for specific IgE are available for most high molecular weight allergens, and a few low molecular weight agents but there are few standardised allergens commercially available which limits their use. A positive test denotes sensitisation, which can occur with or without disease
- the diagnosis of occupational asthma can usually be made without specific bronchial provocation testing, considered to be the gold standard diagnostic test
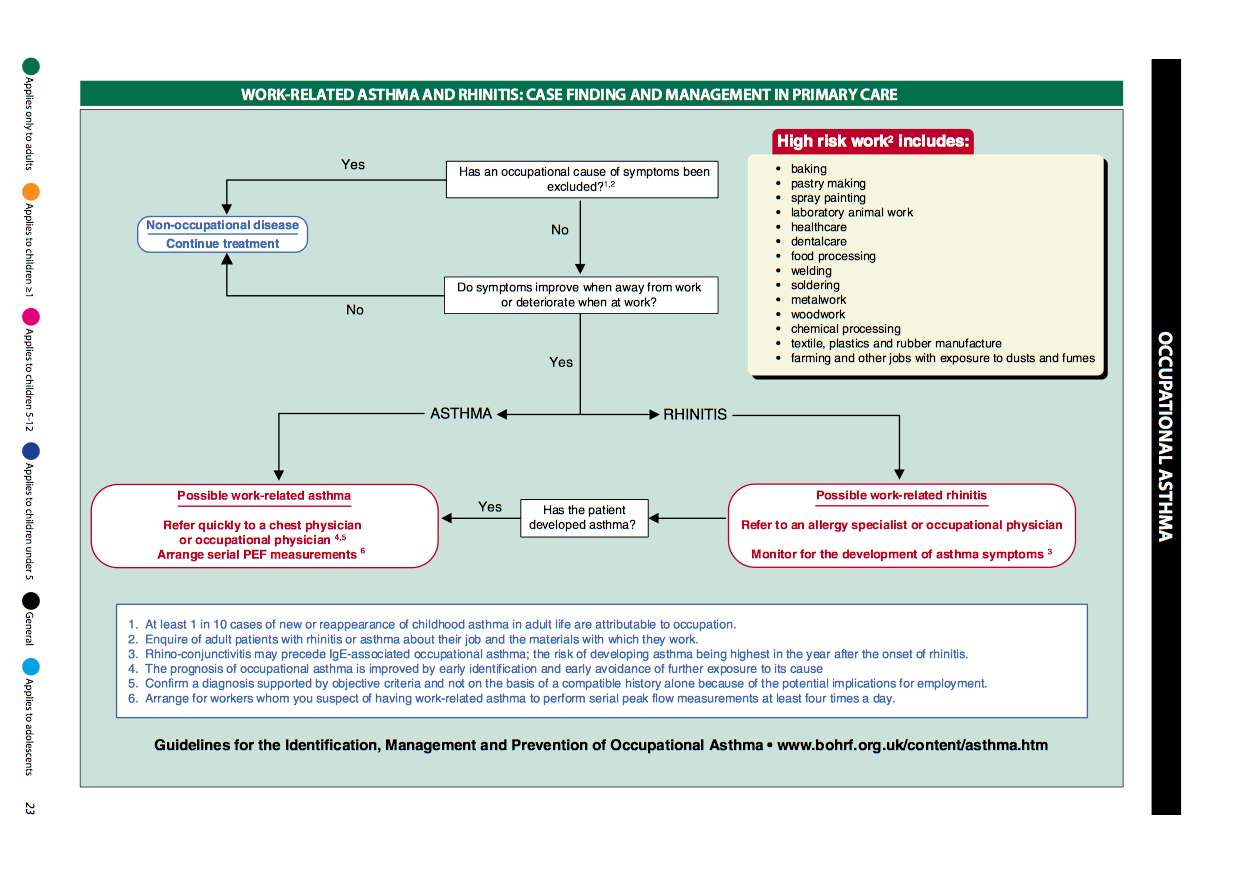
Work-related asthma and rhinitis: case finding and management in primary care (4):
1 in 10 recurrences of asthma in adults are due to occupational asthma, so take a detailed history if important. If a patient has rhinitis which is worsened by being at work, they have a higher risk of asthma starting in the 1st year of symptoms. Occupational asthma has a worse prognosis if there is continued exposure, so prompt diagnosis is important. Advise serial PEF readings (at least 4 a day) and prompt referral to a respiratory specialist. The following chart is helpful:
management principles:
- primary prevention aims to prevent the onset of disease, often by reducing or eliminating exposure to the agent in the workplace
- is the most effective measure
- relocation away from exposure should occur as soon as diagnosis is confirmed, and ideally within 12 months of the first work-related symptoms of asthma (2)
- reduction in airborne exposure will result in a reduction the number of workers who become sensitised and who develop occupational asthma (1)
- secondary prevention aims to detect disease at an early or presymptomatic stage for example by health surveillance
- tertiary prevention aims to prevent worsening symptoms by early recognition and early removal from exposure and is considered later under the management of an identified case of occupational asthma
- referral from primary care:
- if possible work-related asthma
- refer quickly to a chest physician or occupational physician
- arrange serial PEF measurements
- if possible work-related rhinitis
- refer to an allergy specialist or occupational physician
- monitor for the development of asthma symptom
For more information then consult the British Occupational Health Research Foundation http://www.bohrf.org.uk/
Reference:
- (1) Guidelines for the prevention, identification & management of occupational asthma: Evidence review & recommendations. British Occupational Health Research Foundation. London. 2010
- (2) British Thoracic Society (BTS)/Scottish Intercollegiate Guidelines Network (SIGN) 2011. British Guideline on the Management of Asthma. A national clinical guideline
- (3) Fishwick D et al. Standards of care for occupational asthma. Thorax. 2008;63(3):240-50.
- (4) British Thoracic Society (BTS)/Scottish Intercollegiate Guidelines Network (SIGN) 2019.. British Guideline on the Management of Asthma. A national clinical guideline
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.