Assessing childhood depression in primary care
Last reviewed dd mmm yyyy. Last edited dd mmm yyyy
Assessing the severity of depression (in children and young people) in primary care:
Consider the ICD-10 definitions of depression:
- Mild depression: four symptoms
- Moderate depression: five or six symptoms
- Severe depression: seven or more symptoms, with or without psychotic features
Key symptoms
- at least one of the following symptoms are present on most days, most of the time, for at least 2 weeks
- persistent sadness or low (irritable)** mood
- loss of interests and/or pleasure
- fatigue or low energy
If any key symptoms are present, ask about associated symptoms
- poor or increased sleep
- poor concentration or indecisiveness
- low self-confidence
- poor or increased appetite
- suicidal thoughts or acts
- agitation or slowing of movements
- guilt or self-blame
In the assessment and treatment of depression in children and young people, special attention should be paid to the issues of (2):
- confidentiality
- the young person's consent (including Gillick competence)
- parental consent
- child protection
- the use of the Mental Health Act in young people
- the use of the Mental Capacity Act in young people
- the use of the Children Act
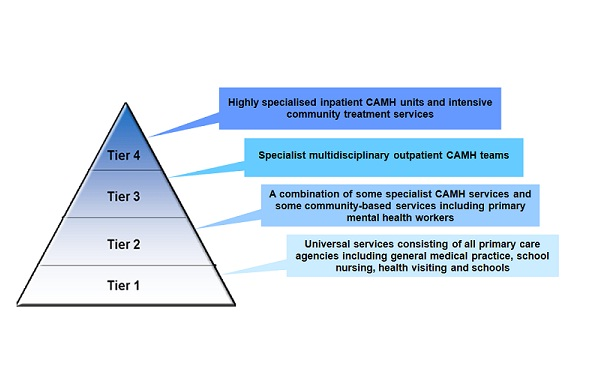
Factors for referral to tier 1
- exposure to a single uncomplicated undesirable event in the absence of other risk factors for depression
- exposure to a recent undesirable life event in the presence of two or more other risk factors with no evidence of depression and/or self-harm
- exposure to a recent undesirable life event in the context of multiple-risk histories for depression in one or more family members (parents or children) providing that there is no evidence of depression and/or self-harm
- mild depression without comorbidity
Factors for referral to CAMHS tier 2 or 3
- depression with two or more other risk factors for depression
- depression where one or more family members (parents or children) have multiple-risk histories for depression
- mild depression in those who have not responded to interventions in tier 1 after 2-3 months
- moderate or severe depression (including psychotic depression)
- signs of a recurrence of depresion in those who have recovered from previous moderate or severe depression
- unexplained self-neglect of at least 1 month's duration that could be harmful to their physical health
- active suicidal ideas or plans
- referral requested by a young person or their parent(s) or carer(s)
Factors for referral to CAMHS tier 4
- high recurrent risk of acts of self-harm or suicide
- significant, ongoing self-neglect (for example, poor personal hygiene, or significant reduction in eating that could be harmful to the physical health of the child/young person)
- intensity of assessment/treatment and/or level of supervision that is not available in tiers 2/3.
Notes:
- Tier 1
- primary care services including GPs, paediatricians, health visitors, school nurses, social workers, teachers, juvenile justice workers, voluntary agencies and social services
- primary care services including GPs, paediatricians, health visitors, school nurses, social workers, teachers, juvenile justice workers, voluntary agencies and social services
- Tier 2 CAMHS
- services provided by professionals relating to workers in primary care including clinical child psychologists, paediatricians with specialist training in mental health, educational psychologists, child and adolescent psychiatrists, child and adolescent psychotherapists, counsellors, community nurses/nurse specialists and family therapists
- services provided by professionals relating to workers in primary care including clinical child psychologists, paediatricians with specialist training in mental health, educational psychologists, child and adolescent psychiatrists, child and adolescent psychotherapists, counsellors, community nurses/nurse specialists and family therapists
- Tier 3 CAMHS
- specialised services for more severe, complex or persistent disorders including child and adolescent psychiatrists, clinical child psychologists, nurses (community or inpatient), child and adolescent psychotherapists, occupational therapists, speech and language therapists, art, music and drama therapists, and family therapists
- specialised services for more severe, complex or persistent disorders including child and adolescent psychiatrists, clinical child psychologists, nurses (community or inpatient), child and adolescent psychotherapists, occupational therapists, speech and language therapists, art, music and drama therapists, and family therapists
- Tier 4 CAMHS
- tertiary-level services such as day units, highly specialised outpatient teams and inpatient units
** Whilst this is a well-documented feature it is not currently listed in ICD-10 diagnostic criteria.
Reference:
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.