Cause of death statement on death certicate (Part I and Part II)
Last reviewed dd mmm yyyy. Last edited dd mmm yyyy
CAUSE OF DEATH STATEMENT
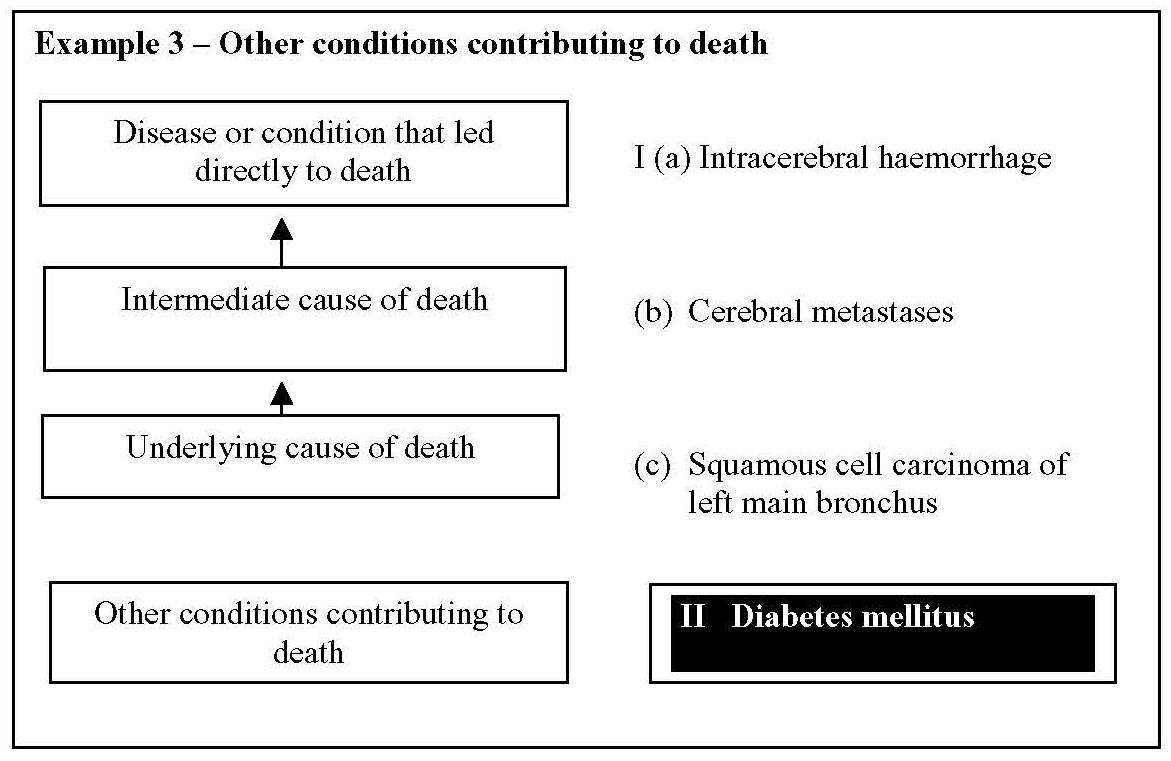
This section of the certificate is divided in Parts I and II. Part I is used to show the immediate cause of death and any underlying cause or causes. Part II should be used for any significant condition or disease that contributed to the death but which is not part of the sequence leading directly to death.
Part I
- It is essential that you state the cause(s) of death accurately and fully to the best of your knowledge and belief. The death certificate is the relatives' permanent legal record of the death. The mortality statistics derived from the death certificate are vital for public health surveillance and other purposes
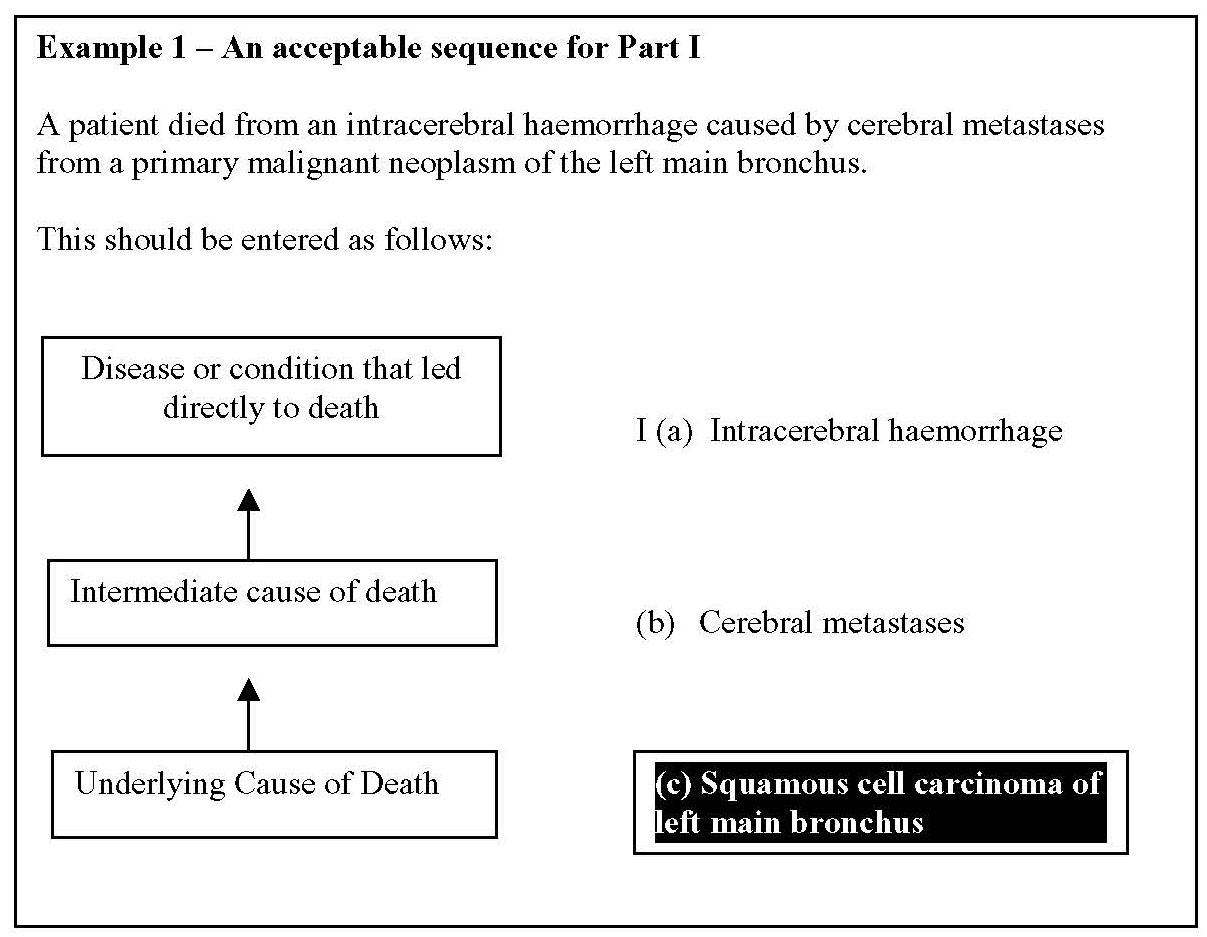
- underlying cause of death - you should approach this by considering the main causal sequence of conditions leading to death. You should state the disease or condition that led directly to death on the first line [I(a)] and work your way back in time through the antecedents of this condition until you reach the Underlying Cause of Death, which initiated the chain of events leading ultimately to death. The lowermost completed line in Part I should therefore contain the Underlying Cause of Death.
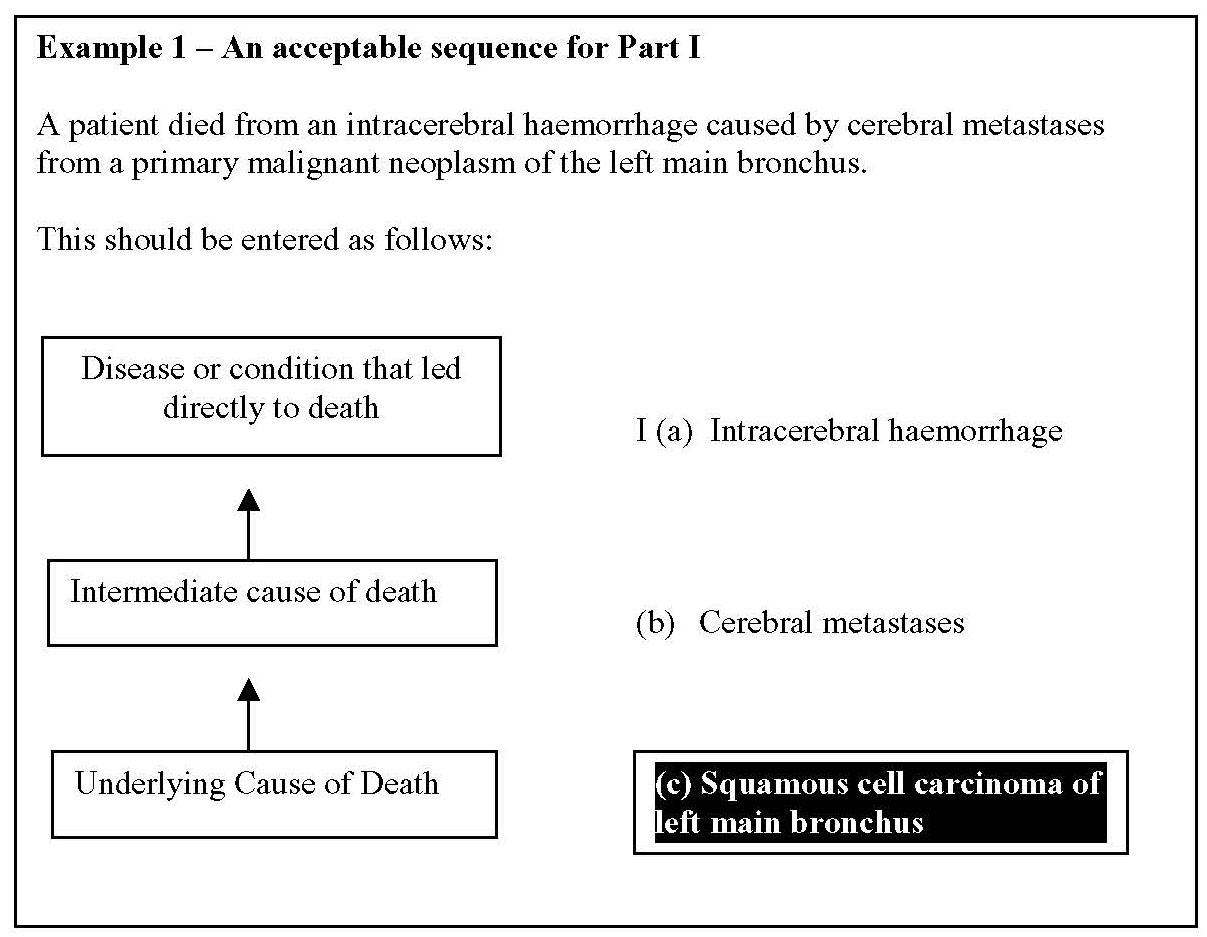
The Underlying Cause of Death in this case is squamous cell carcinoma of the left main bronchus
- for some deaths there may be only one condition which led directly to death with no antecedents, e.g. subarachnoid haemorrhage or meningococcal meningitis. In this case it is perfectly acceptable to complete only line [I(a)]
- your statement of the cause of death should be as specific as your information allows. For example, when recording a neoplasm state the histopathology, whether malignant or benign, the anatomical site, whether primary or secondary and, for the latter, the site of the primary and date of removal if known. In Example 1, cerebral metastases resulting from squamous cell carcinoma of the left main bronchus is given, rather than simply lung cancer
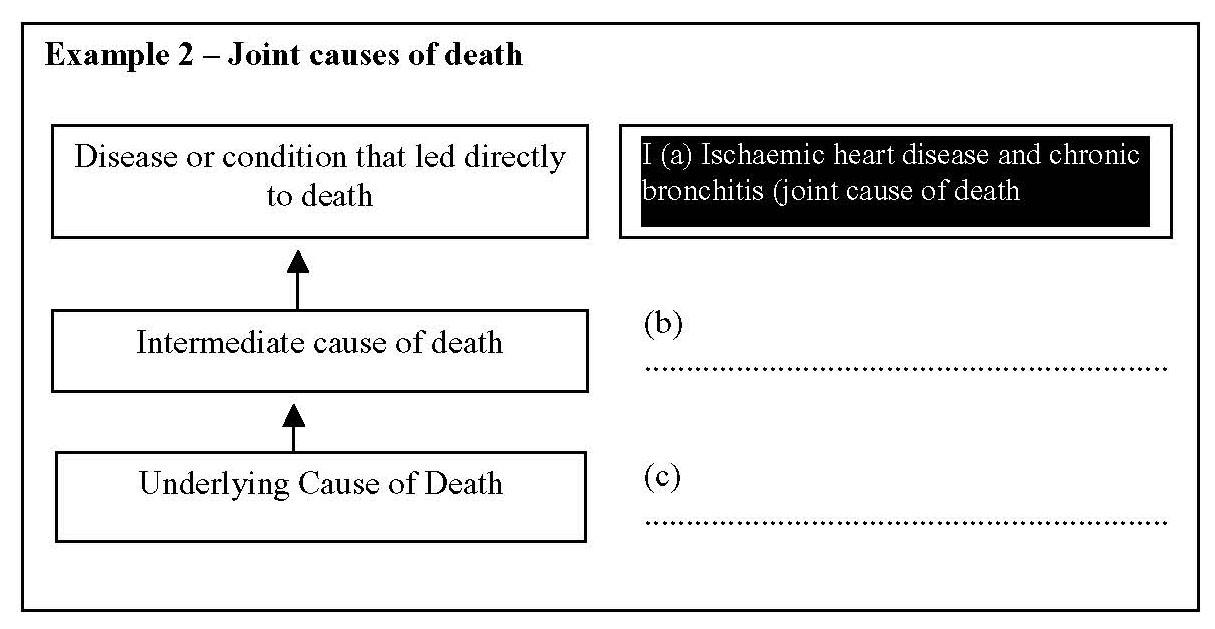
- joint causes of death - sometimes there are apparently two distinct conditions leading to death. If there is no way of choosing between them, they should be entered on the same line indicating in brackets that they are joint causes of death. In such cases, the first condition will be taken as the Underlying Cause of Death for coding purposes.
- Smoking - inclusion of the term 'smoking' is acceptable if accompanied by a medical cause of death
Avoid organ failure alone
- do not certify deaths as due to the failure of any organ, without specifying the disease or condition that led to the organ failure. Failure of most organs can be due to unnatural causes, such as poisoning, injury or industrial disease. This means that the death will have to be referred to the coroner if no natural disease responsible for organ failure is specified. Examples:
- Ia. Renal failure
- Ib. Necrotising-proliferative nephropathy
- Ic. Systemic lupus erythematosus
- II. Raynaud's phenomenon and vasculitis
- Ia. Liver failure
- Ib. Hepatocellular carcinoma
- Ic. Chronic Hepatitis B infection
- Ia. Congestive cardiac failure
- Ib. Essential hypertension
- conditions such as renal failure may come to medical attention for the first time in frail, elderly patients in whom vigorous investigation and treatment may be contraindicated, even though the cause is not known. When such a patient dies, you are advised to discuss the case with the coroner before certifying. If the coroner is satisfied that no further investigation is warranted, the registrar can be instructed to register the death based on the information available on the death certificate. The registrar cannot accept an death certificate that gives only organ failure as the cause of death, without instruction from the coroner
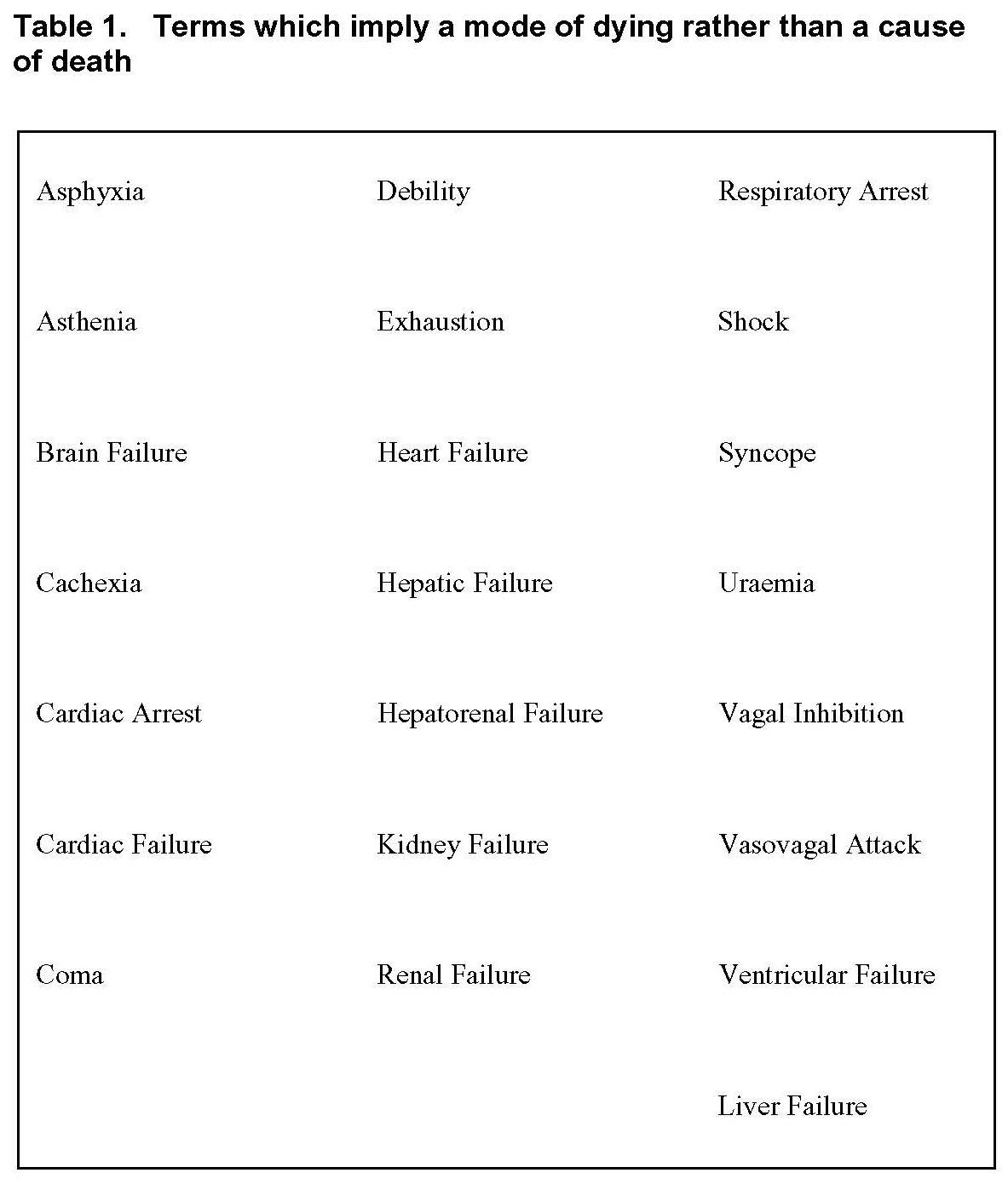
Avoid terminal events, modes of dying and other vague terms
- Terms that do not identify a disease or pathological process clearly are not acceptable as the only cause of death. This includes terminal events, or modes of dying such as cardiac or respiratory arrest, syncope or shock. Very vague statements such as cardiovascular event or incident, debility or frailty are equally unacceptable. 'Cardiovascular event' could be intended to mean a stroke or myocardial infarction. It could, however, also include cardiac arrest or fainting, or a surgical or radiological procedure. If no clear disease can be identified as the cause of death, referral to the coroner will be necessary
- Old age, senility
- see linked item below
Part II
Part II should be used when one or more conditions have contributed to death but are not part of the main causal sequence leading to death. Part II should not be used to list all conditions present at death. For example, diabetes mellitus may have hastened the death of the patient in Example 1
In this case, the certificate should be completed as follows:
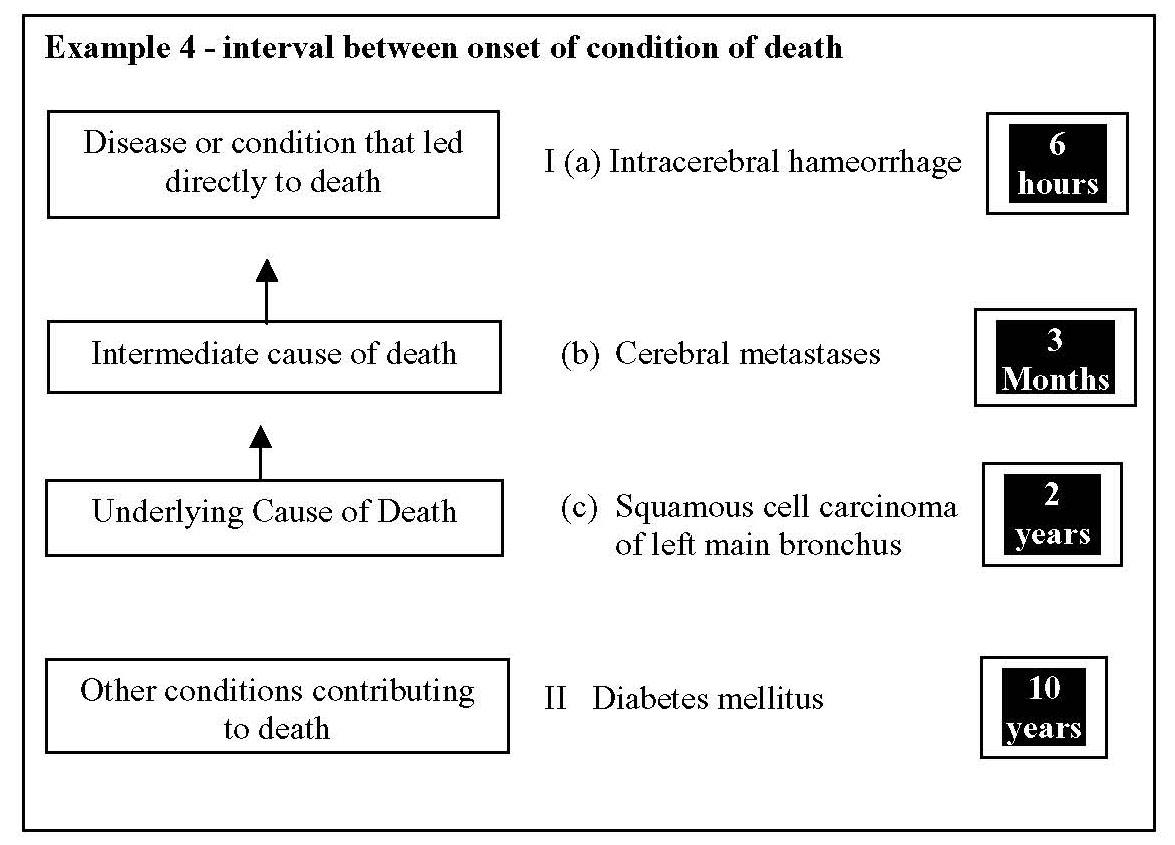
Interval between onset of conditions and death - if possible, it is also important to state the approximate interval between the onset of each condition and death for Parts I and II, as this information is used for coding purposes. For example, the following intervals might be appropriate
General points
- where appropriate in Part I and II, you should give information about clinical interventions, procedures or drugs that may have led to adverse affects
- if you use a term such as 'cerebrovascular accident', which may be misinterpreted by a lay person as implying violence, take care to explain it to the relatives
- avoid abbreviations such as CVA, MI or PE on the certificate. This also applies to medical symbols. Inclusion of such ambiguous terms may delay registration
- bronchopneumonia is a common terminal event in patients with a major chronic illness. Do not write bronchopneumonia as the sole cause of death if another condition(s) can be identified as the Underlying Cause of Death
Reference:
- Manchester City Council (2007). Death Certification Guidance for doctors certifying cause of death.
- Southampton University Hospitals NHS Trust (Accessed 22/6/12). Medical Certificate of Cause of Death Notes for Doctors
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.