Type 1 diabetes and intercurrent illness
Last reviewed dd mmm yyyy. Last edited dd mmm yyyy
This guideline is not intended to serve as a protocol or standard of care:
- this is best practice based on all clinical data available for an individual case and may be subject to change as scientific knowledge and technology advances and patterns of care evolve. Adherence to guideline recommendations will not ensure a successful outcome in every case, nor should it be construed as including all proper methods of care or excluding other acceptable methods of care aimed at the same result. Ultimately a judgement must be made by the appropriate healthcare professional(s) responsible for a particular clinical procedure or treatment plan following discussion with the patient, covering the diagnostic and treatment options available. It is advised that any significant departure from the guideline should be documented in the patient’s medical record at the time the decision is taken.
Examples of intercurrent illness where "sick day rules" would be considered (1):
The following list of such illnesses is not exhaustive:
- the common cold
- influenza
- coronavirus
- diarrhoea and vomiting
- urinary tract infection
- chest infection
- pneumonia
- abscess
- injury (e.g. fracture)
General advice for managing diabetes during intercurrent illness (1)
S (Sugar)
- Blood glucose levels can rise during illness even if the person is not eating
- Advise to increase blood glucose monitoring if the person has access to it
- Diabetes medications (sulfonylureas and insulin doses) may need to be increased temporarily during illness to manage these raised glucose levels
I (Insulin)
- NEVER stop insulin or oral diabetes medications*
- Insulin doses may need to be increased during illness, especially if ketones are present
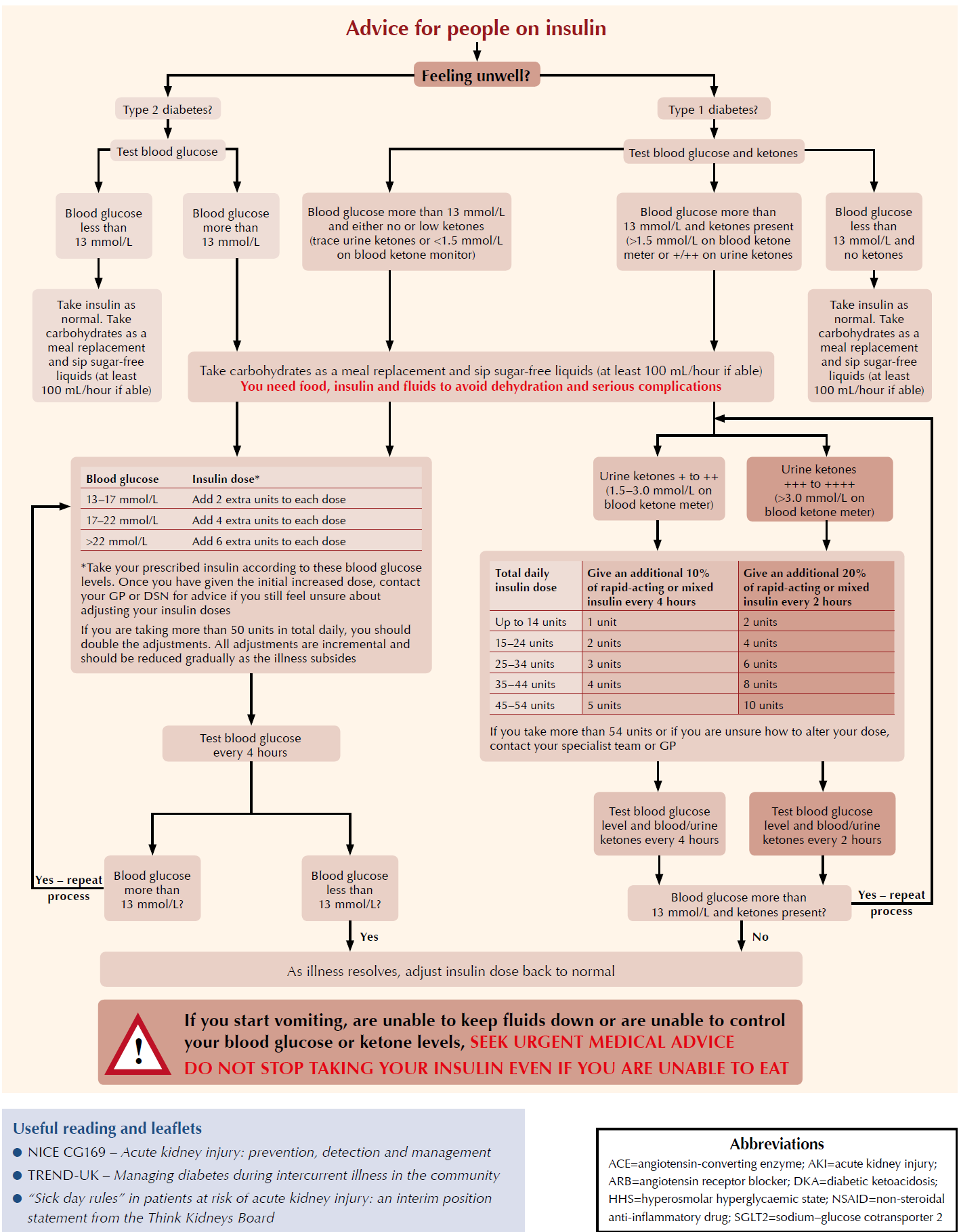
- Specific advice for people on insulin therapy is presented below
C (Carbohydrate)
- Ensure the person maintains hydration and carbohydrate intake
- If the person is not able to eat or is vomiting, advise to replace meals with sugary fluids
- If blood glucose levels are high, maintain fluid intake with sugar-free fluids
- If blood glucose levels are low, encourage regular intake of sugary fluids
K (Ketones)
- In type 1 diabetes, advise to check for ketones every 2–4 hours
- Give extra rapid-acting insulin doses (in addition to regular doses) based on total daily
- insulin dose if ketones are present – see insulin algorithm below
- Advise to drink plenty of water to maintain hydration and flush through ketones
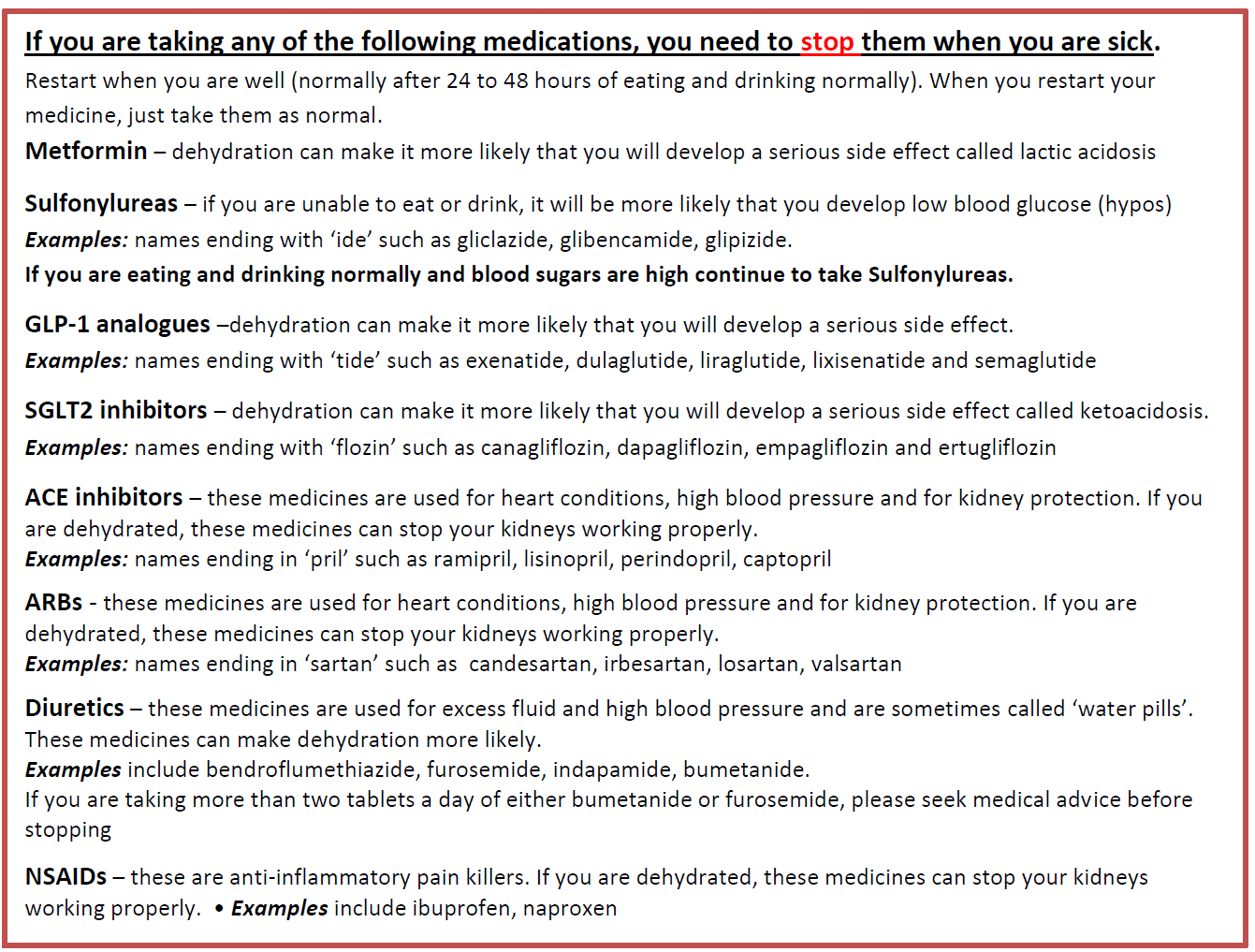
Medications that Type 1Diabetics should stop if unwell (4):
TYPE 1 DM
Encourage adequate dietary and fluid intake:
- maintain an adequate fluid intake of approximately 1 glass (100-200ml) of sugar-free liquids every hour
- maintain a regular intake of carbohydrate - if unable to take solid foodstuffs, but tolerating fluids, encourage the person to take carbohydrate in other forms i.e. soup, fruit juice, milk or milky drinks, such as hot chocolate
- as a last resort, advise the person to replace carbohydrate in liquid form i.e. ordinary, non-diet cola or lemonade
- if occasional vomiting or nauseated, consider the use of an anti-emetic
- consider providing an electrolyte replacement, e.g. Dioralyte®, Rehidrat®, Electrolade® (also appropriate if person is experiencing significant diarrhoea)
- if, however, the person is unable to swallow or keep fluids down for any length of time (i.e. > 4 hours), hospital admission may be appropriate
- aim to drink at least 3 L of fluid (5 pints) a day to prevent dehydration (3)
- if vomiting or diarrhoea is persistent, they should seek immediate medical advice as intravenous fluids may be required.
Increase frequency of blood glucose (BG) monitoring and test for ketones:
- increase blood glucose monitoring to at least 4 hourly; if moderate to large ketones (1.5 - > 3 mmol/l) are present, BG testing should be carried out 2 hourly
- ensure that glucose and ketone monitoring equipment is accurate (QC (quality control) has been carried out recently), strips are in date and, as far as possible, that the person's self-testing technique is accurate
- ensure that glucose and ketone monitoring equipment is accurate (QC (quality control) has been carried out recently), strips are in date and, as far as possible, that the person's self-testing technique is accurate
- ketone testing should also be carried out 2-4 hourly, whether by testing urine or utilising Optium beta-ketone test strips with an Xceed meter or LX Ketone sensor with a Glucomen LX meter
- specialist and community health care professionals should arrange to review results with the patient on a very regular basis to avoid, where possible, the need for hospital admission
A schemata has been suggested (1):
Admission or specialist advice (2,3)
The decision to admit a person or seek specialist advice will depend on clinical judgement, taking into account the person's age, underlying illness(es) and complications, and the presence of hyperglycaemia and ketosis.
- immediate hospital admission is indicated if:
- an immediate risk of DKA
- is moderate ketonuria (2+ on urine dipstick) or ketonaemia (1.5–2.9 mmol/L) with or without hyperglycaemia and the person cannot eat or drink, as there is a risk of DKA.
- person does not improve rapidly with insulin treatment
- blood glucose persistently >20 mmol/L despite best therapy (2)
- suspicion of underlying diagnosis that requires hospital admission (eg, myocardial infarction, intestinal obstruction)
- patient is unable to manage adjustment of normal diabetes care
- patient lives alone, has no support and may be at risk of slipping into unconsciousness
- clinical signs of ketosis or worsening condition (eg, Kussmaul's respiration, severe dehydration, abdominal pain)
- consider hospital admission or seeking urgent specialist advice if:
- underlying condition is unclear
- person is dehydrated or at risk of dehydration.
- Vomiting persists beyond 2 hours.
- person and their family/carers are unable to keep the blood glucose level above 3.5 mmol/L.
- person is on continuous subcutaneous insulin pump therapy
Further information on coping during a period of illness for people with type 1 diabetes is available on the Diabetes UK website (www.diabetes.org.uk).
Reference:
- Down S. How to advise on sick day rules. Diabetes & Primary Care (2018); 20 (1): 15-16.
- Patient.co.uk (Accessed 8/5/2020).Diabetes and Intercurrent Illness.
- CKS (Accessed 8/5/2020). Type 2 Diabetes.
- NHS Sandwell and West Birmingham CCG (Accessed 23/9/2020). Sick day rules for patients on multiple daily injections (MDI) OR PUMP THERAPY: how to manage Type 1 diabetes if you become unwell with coronavirus.
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.