Investigation in testosterone deficiency
Last reviewed dd mmm yyyy. Last edited dd mmm yyyy
Blood tests - measurement of morning basal testosterone, LH, FSH, PRL - measurement of the basal levels of testosterone, LH and FSH will allow distinction between gonadal disease and hypothalamic-pituitary disease (1)
- primary hypogonadism - elevated gonadotrophin levels and low testosterone levels
- secondary hypogonadism - low to normal gonadotrophin levels and low testosterone levels
When considering a diagnosis of symptomatic TD, other blood investigations should include:
- haematocrit as part of FBC
- prostate specific antigen (PSA), with appropriate counselling
- Appropriate tests according to physical findings and to determine cardiovascular risk
Total testosterone (TT) should be measured before 11am (2,3) with a reliable method, on at least two separate occasions,(3) preferably 4 weeks apart. Fasting levels should be obtained where possible, (3)as non-fasting levels may be up to 30% lower (3)If TT is low or borderline (<12 nmol/L):
- Measure sex hormone-binding globulin to calculate free testosterone (FT: an online FT calculator and downloadable app, sponsored by the Primary Care Testosterone Advisory Group, can be found at: http://www.pctag.uk/testosterone-calculator/)
- Measure serum luteinising hormone (LH) to differentiate primary from secondary TD.
- Measure follicle stimulating hormone (FSH) if fertility is an issue
Biopsy of the testes may be necessary for diagnosis but rarely reveals a treatable pathology.
Other investigations may be indicated and include:
- skull radiology including a pituitary CT scan
- semen analysis
- chromosomal analysis e.g. Klinefelter's disease
- bone age estimation
Asuggested algorithm for assessment of possible testosterone deficiency in primary care (1):
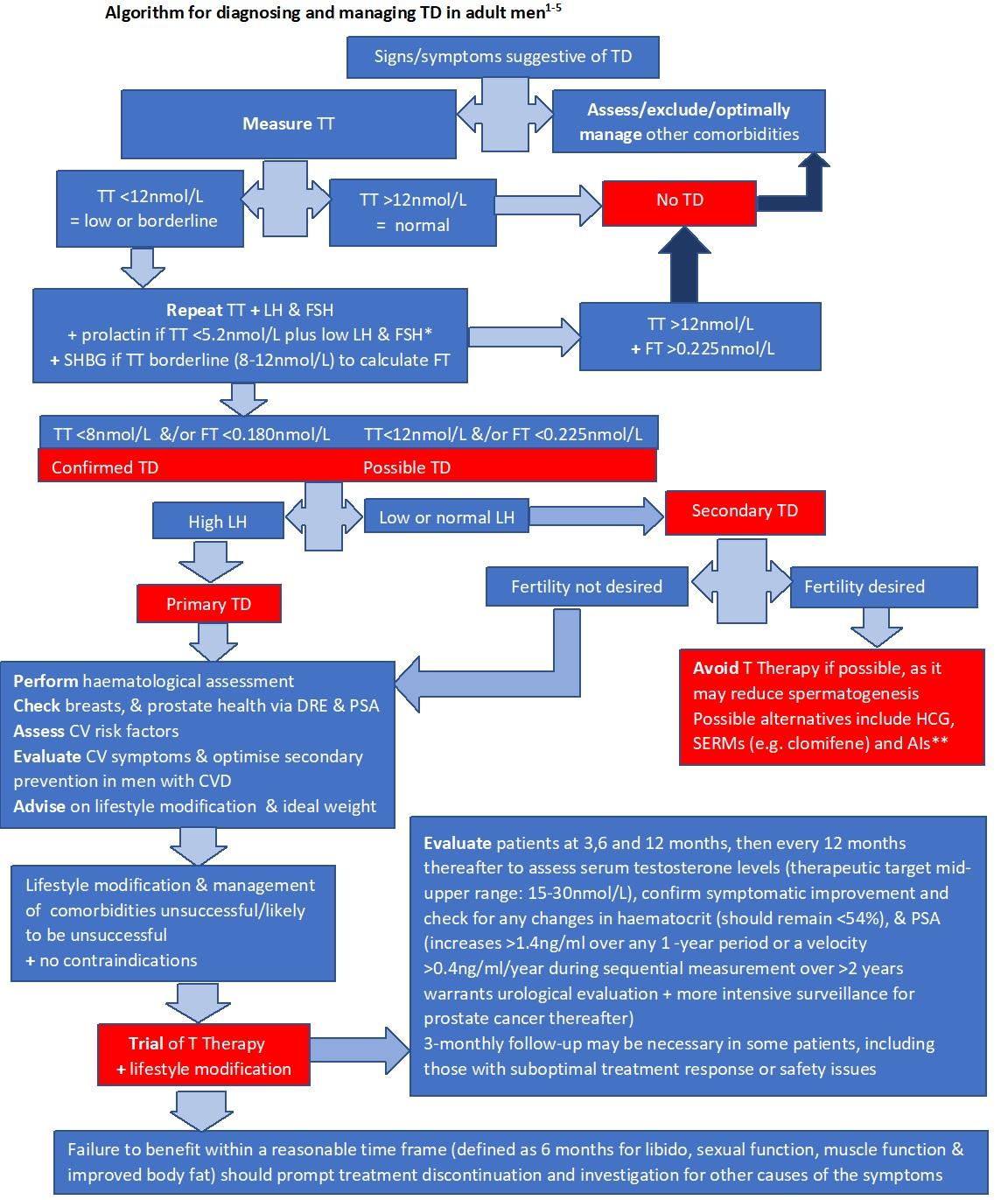
- Key points (contributor: Professor Mike Kirby 5/6/2018):
- an acute illness may cause a fall in testosterone levels, therefore investigate suspected testosterone deficiency once any acute illness has fully resolved
- most discriminant symptoms associated with low testosterone (<12nmol/L) are: low libido, loss of early morning erections & erectile dysfunction - particularly in combination
- consider potentially reversible factors that may be causing a low testosterone, that can be addressed - concurrent illness, certain drugs (prescribed or otherwise e.g. ketoconazole, cimetidine, spironolactone, chemotherapy, opioids) and lifestyle factors (e.g. excessive alcohol; stress; significant weight gain/obesity, excessive exercise etc.).
- an acute illness may cause a fall in testosterone levels, therefore investigate suspected testosterone deficiency once any acute illness has fully resolved
Reference:
- Lunenfeld B, Mskhalaya G, Zitzmann M, et al. Recommendations on the diagnosis, treatment and monitoring of hypogonadism in men. Aging Male 2015;18:5-15.
- Dohle GH, Arver S, Bettochi C et al. Guidelines on Male Hypogonadism. European Association of Urology 2017. Available at: http://uroweb.org/guideline/male-hypogonadism/ (Accessed May 2018).
- Caronia LM, Dwyer AA, Hayden D, et al. Abrupt decrease in serum testosterone levels after an oral glucose load in men: implications for screening for hypogonadism. Clin Endocrinol (Oxf) 2013;78:291-296.
- Lehtihet M, Arver S, Bartuseviciene I, et al. S-testosterone decrease after a mixed meal in healthy men independent of SHBG and gonadotrophin levels. Andrologia 2012;44:405-410.
- British Society of Sexual Medicine. Guidelines on the management of sexual problems in men: the role of androgens 2010. Available at: http://bssmorguk.ipage.com/wpcontent/ uploads/2017/05/UK_Guidelines_Androgens_Male_2010.pdf (Accessed May 2018).
Related pages
Create an account to add page annotations
Annotations allow you to add information to this page that would be handy to have on hand during a consultation. E.g. a website or number. This information will always show when you visit this page.